The Characteristics and Survival Outcomes in Patients Aged 70 Years and Older with Nasopharyngeal Carcinoma in the Intensity-Modulated Radiotherapy Era
Article information
Abstract
Purpose
We aim to examine nasopharyngeal carcinoma (NPC) characteristics and survival outcomes in patients aged 70 years and older in the intensity-modulated radiotherapy (IMRT) era.
Materials and Methods
From 2006 to 2013, 126 non-metastatic NPC patients aged ≥ 70 years who were treated with IMRT +/‒ chemotherapy were included. Adult Comorbidity Evaluation 27 (ACE-27) was used to measure patient comorbidities. The overall survival (OS) and cancer-specific survival (CSS)were calculatedwith the Kaplan-Meier method, and differenceswere compared using the log-rank test. The Cox proportional hazards model was used to carry out multivariate analyses.
Results
For the entire group, only two patients (1.6%) presented stage I disease, and up to 84.1% patients had stage III-IVB disease. All patients had a comorbidity score of 0 in 24 (19.0%), 1 in 45 (35.7%), 2 in 42 (33.3%), and 3 in 15 (11.9%) patients. The main acute grade during radiotherapy was 3-4 adverse events consisting of mucositis (25.4%), bone marrow suppression (16.7%), and dermatitis (8.7%). After treatment, four patients (3.2%) developed temporal lobe injury. Five-year CSS and OS rates were 67.3% (95% confidence interval [CI], 58.6% to 77.4%) and 54.0% (95% CI, 45.6% to 63.9%), respectively. Five-year OS was significantly higher for ACE-27 score 0-1 than ACE-27 score 2-3 (72.9% and 39.9%, respectively; p < 0.001). Multivariate analyses showed ACE-27 score 0-1 was significantly associated with superior OS (hazard ratio [HR], 3.02; 95% CI, 1.64 to 5.55; p < 0.001). In addition, the rate of OS was higher for stage I-III than that of stage IV, with borderline significance (HR, 1.67; 95% CI, 0.99 to 2.82; p=0.053). But no significant advantage was observed in OS when chemotherapy was used (p > 0.05).
Conclusion
Our findings suggest IMRT +/– chemotherapy has a manageable toxicity and provides an acceptable survival in patients aged ≥ 70 years with NPC. ACE-27 score was significantly associated with survival outcomes in this group population.
Introduction
Nasopharyngeal carcinoma (NPC) disproportionately burdens East and Southeast Asia accounting for two-thirds of new cases worldwide [1]. Among new cases, 40% are in China, with the highest prevalence in Southern China [1]. The relative risk of NPC increases with age and peaks at approximately 55 years of age and begins to decline at ages > 60 years [2]. However, the old-age ratio (total number of individuals aged ≥ 65 years per 100 working age people [20-64 years]) is projected to rise from 13 elderly people per 100 in 2010 to 45 per 100 by 2050 [3]. Moreover, the population of individuals aged 70 years and older are rising from approximately 75 million in 2010 to a projected 225 million by 2050 [3]. The number of elderly patients with NPC will increase with the rapidly growing elderly population in China, and therefore essential to the management of this population, defined in the present study as individuals aged ≥ 70 years.
Patients ages 70 years and older are often excluded from studies, especially clinical trials due to age exclusion [4,5]. Considering the lack of clinical trials for this group of patients, the treatment for these patients generally follows guidelines tailored for adult patients (age range, 18 to 69 years). Recently, several studies selected patients that were ages 60 to 65 years as a cutoff point for elderly NPC [6-8]. However, this choice may not be completely reasonable, since the physical health among those ages 60-65 years is improving among the general population. In contrast, patients older than 70 years may vastly differ from adults [9,10], for which closer association with multiple comorbidities, poorer performance status, reduced organ reserve, and less social support. For these reasons, the treatment of patients ages 70 years and older warrants further research.
Furthermore, intensity-modulated radiotherapy (IMRT) is slowly replacing two-dimensional conventional radiotherapy (2DRT) as the primary radiotherapy (RT). However, to date, there are no prior studies among patients ages 70 years and older that investigated characteristics and survival outcomes of patients treated with IMRT. Thus, this study aims to fill multiple knowledge gaps by evaluating NPC treatment among patients aged ≥ 70 years in the IMRT era.
Materials and Methods
1. Patient characteristics
We conducted a retrospective review of case records for patients with NPC treated at Sun Yat-sen University Cancer Center (SYSUCC) from January 2006 to December 2013. Patients included in the analysis were aged ≥ 70 years, histologically proven NPC, non-metastatic, and treated with IMRT. In all, 126 patients were included in the study. Key raw data was uploaded onto the Research Data Deposit (RDD) public platform (http://www.researchdata.org.cn), with the approval RDD number as RDDA2017000334 to validate the authenticity of this article.
2. Clinical staging and co-morbidity assessment
Patients had undergone pretreatment evaluation comprising of physical examination, hematology and biochemistry profiles, as well as obtained patient complete history information. Additionally, patients also underwent nasopharynx and neck magnetic resonance (MR) imaging, chest X-ray, or computed tomography (CT), CT whole-body bone scan single photon emission, and abdominal ultrasonography. We performed positron emission tomography‒computed tomography on 25 of 126 patients (19.8%). We restaged patients according to guidelines set by the seventh edition of the American Joint Commission on Cancer staging [11]. Moreover, Adult Comorbidity Evaluation 27 (ACE-27) was performed for identifying important medical comorbidities and assess severity among elderly patients [12].
3. Radiotherapy
While immobilized in the supine position using a thermoplastic head and shoulder mask, all patients received IMRT. Contrast-enhanced planning CT (3 mm-slice thickness) images from the superior border of frontal sinus to two centimeters below sternoclavicular joint were obtained. Information obtained were transferred to the Monaco treatment planning system (ver. 3.02, Elekta AB, Stockholm, Sweden). The IMRT plan was designed based on previous studies [13], and in accordance with the International Commission on Radiation Units (ICRU) and Measurements Reports 62 [14] and 83 [15].
4. Chemotherapy and other treatments
Chemotherapy is required for treatment of locally advanced diseases; however, chemotherapy was not given to some patients due to patient refusal or suggesting intolerance to chemotherapy. The most commonly used regimens for neoadjuvant chemotherapy were cisplatin (80 mg/m2) with docetaxel (80 mg/m2) for every 3 weeks or cisplatin (80 mg/m2) with 5-fluorouracil (800 mg/m2/day over 120 hours). Concurrent chemotherapy consisted of cisplatin (80 or 100 mg/m2) on weeks 1, 4, and 7 of radiotherapy, or cisplatin (40 mg/m2) weekly. Modification of dosage was performed, if necessary, at the doctors’ discretion. In addition, there were patients that received other therapies besides chemotherapy (n=11). Seven patients underwent targeted therapy concurrent with IMRT, consisting of two by cetuximab and five by nimotuzumab. Another four patients received primary tumor brachytherapy with CT-guided permanent implantation of 125I seeds after IMRT.
5. Image assessment of temporal lobe injury
In the present study, a diagnosis of temporal lobe injury (TLI) was based on follow-up MR images. We must also note that the diagnosis of TLI was based on the criteria described by Wang et al. [16]. The criteria used were as follow: (1) white matter lesions were defined as areas of finger-like lesions of increased signal intensity on T2-weighted images in the temporal lobe; (2) contrast-enhanced lesions were defined as lesions with or without necrosis on post-contrast T1-weighted images with heterogeneous signal abnormalities on T2-weighted images; and (3) determined cysts as round or oval well-defined lesions of very high signal intensity on T2-weighted images with a thin or imperceptible wall.
6. Follow-up and statistical analysis
During IMRT, we evaluated patients at least once a week. After 1 month of RT completion, the first assessment of response to treatment was performed. Afterwards, every 3 months during the first 3 years patient evaluation was performed. Thereafter, every 6 months for the following 2 years, and annually afterwards. We measured survival times as the initial start of RT to last follow-up visit or date of the event. Overall survival (OS) was measured as the period from first RT treatment to the last follow-up visit or date of death. We defined cancer-specific survival (CSS) as the period from initial RT treatment to the date of death as a result of NPC or the last follow-up visit.
Kaplan-Meier method was used to calculate actuarial rates, and the differences were compared using the log-rank test. Covariates including age, sex, ACE-27 score, N category, T category, overall stage, radiation dose, and chemotherapy were included in all tests. Cox proportional hazards model was performed to carry out multivariate analyses. p-value of < 0.05 was determine statistically significant. R software (ver. 3.2.3) was used to perform all statistical analyses.
7. Ethical statement
The present study was approved by the Institutional Review Board at SYUCC and conducted in compliance with institutional policy to protect patients’ private information.
Results
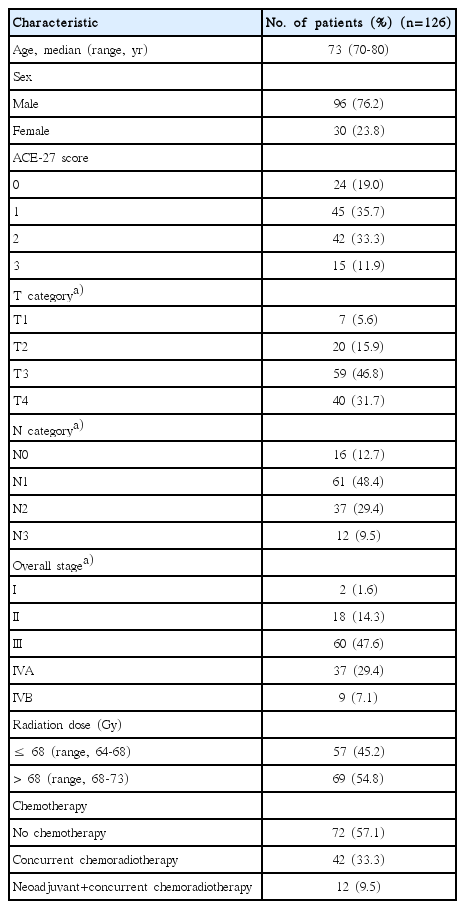
1. Symptoms, signs, and comorbidity before treatment
Table 1 presents patients’ clinical characteristics. Median age at diagnosis was 73 years (ages ranged 70 to 80 years). Among the 126 patients, only two patients (1.6%) had stage I disease, and 84.1% patients presented III/IVA-B disease. The most common symptom was cervical mass with an incidence of 52% (66 patients), followed by nasal problems (55 patients, 44%), auditory problems (46 patients, 37%), and headache (22 patients, 17%). The ACE-27 score for comorbidity was 0 in 24 (19.0%), 1 in 45 (35.7%), 2 in 42 (33.3%), and 3 in 15 (11.9%).
2. Treatment course and toxicity
All patients completed the planned RT. The median radiation dose for primary tumor and regional lymph node were 68.4 Gy (range, 64.2 to 73.4 Gy) and 64.6 Gy (range, 59.6 to 68.4 Gy), respectively. Overall, 72 patients (57%) were treated with RT alone, 42 patients (33%) received concurrent chemoradiation therapy (CCRT), and 12 patients (10%) received neoadjuvant chemotherapy plus CCRT. Mucositis, bone marrow suppression, and dermatitis were the most common acute toxicities where majority developed within grade 1 to 2, and the incidence of grades 3 to 4 acute toxicities were 18.3%, 10.3%, and 6.3%, respectively. During follow-up, four patients (3.2%) developed radiation-induced TLI. Of the four patients, two patients were staged with T4 disease, the other two patients with T3 disease, and no patients with T1-2 disease developed TLI.
3. Prognostic factors and survival
Following a median follow-up of 40.6 months (range, 3 to 101 months), 58 (46%) patients died. Among the patients that died, 36 (62.1%) died from NPC, 5 (8.6%) died of toxicities related to treatment, and 17 (29.3%) died from internal medical diseases that were unrelated to cancer. Of the 17 patients who died because of internal medical disease, eight were chest infection, six cerebral vascular accidents, one because of second malignancies, and two due to other specific causes. Kaplan-Meier analysis of OS and CSS are presented in Fig. 1. Estimated OS and CSS rates at 5 years were 54.0% (95% confidence interval [CI], 45.6% to 63.9%) and 67.3% (95% CI, 58.6% to 77.4%), respectively. ACE-27 score 0-1 was associated with higher 5-year OS in comparison with that of ACE-27 score 0-1 (72.9% and 39.9%, respectively; p < 0.001) (Fig. 2A). The OS was significantly elevated for stage I-III than stage IV (62.1% and 40.1%, respectively; p=0.018) (Fig. 2C). However, we failed to confirm the positive association of chemotherapy (hazard ratio [HR], 1.30; 95% CI, 0.77 to 2.20; p=0.318) (Fig. 2B) and radiation dose (HR, 1.00; 95% CI, 0.59 to 1.70; p=0.999) (Fig. 2D) with OS. Utilizing the Cox proportional hazards model, we observed the ACE-27 score 0-1 was significantly associated with superior OS (HR, 3.02; 95% CI, 1.64 to 5.55; p < 0.001), and stage IV was associated with inferior OS, with borderline significance (HR, 1.67; 95% CI, 0.99 to 2.82; p=0.053) (Table 2).

Survival rate for patients aged ≥ 70 years treated with intensity-modulated radiotherapy +/– chemotherapy. CSS, cancer-specific survival; OS, overall survival.
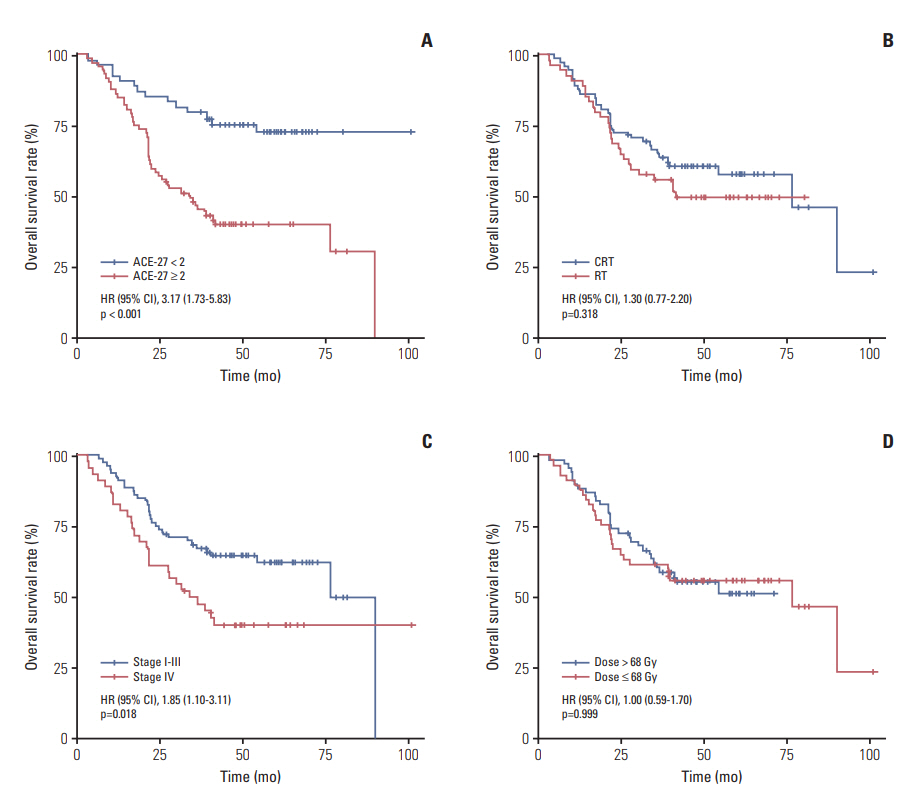
Kaplan-Meier analysis of overall survival is stratified by ACE-27 (A), chemotherapy (B), overall stage (C), and primary tumor dose (D). HR, hazard ratio; CI, confidence interval; ACE-27, Adult Comorbidity Evaluation 27; CRT, chemoradiotherapy; RT, radiotherapy.
4. Prognostic value of chemotherapy in subgroups of NPC patients
Chemotherapy prognostic significance in patients with stage III-IV disease were analyzed. However, stage III-IV diseases did not present a unique patient subgroup, where the addition of chemotherapy to RT was efficacious in improving 5-year OS (56.6% vs. 51.2%, p=0.617) (Fig. 3A). We further analyzed the prognostic value of chemotherapy in the subgroups of patients with NPC with different ACE-27 score. Among patients with ACE-27 score < 2, though the 5-year OS rates (78.0% vs. 69.1%, p=0.554) (Fig. 3B) were higher in patients treated with chemo-radiotherapy than RT alone, this did not reach statistical significance. In contrast, compared with RT alone, chemo-radiotherapy was associated with a trend towards a lower OS for patients with ACE-27 score ≥ 2, with borderline association (50.3% vs. 26.4%, p=0.071) (Fig. 3C).

Kaplan-Meier analysis of overall survival stratified by chemotherapy (RT vs. CRT) in patients with locoregionally advanced nasopharyngeal carcinoma (A), ACE-27 score < 2 (B), and ACE-27 score ≥ 2 (C). HR, hazard ratio; CI, confidence interval; RT, radiotherapy; CRT, chemoradiotherapy; ACE-27, Adult Comorbidity Evaluation 27.
Discussion
To the best of our knowledge, this is the first study on clinical outcomes of patients aged ≥ 70 years with NPC treated by IMRT. The 5-year OS and CSS rates were 54.0% and 67.3%, respectively. Our findings suggest that IMRT +/– chemotherapy provided promising long-term survival in patients aged ≥ 70 years with NPC. Multivariate analyses showed that ACE-27 score 0-1 was significantly associated with superior OS. Additionally, a significant delay in the diagnosis of NPC may exist for patients aged ≥ 70 years, as approximately 84% of elderly NPC patients had stage III-IV disease at presentation, much higher than 70% among adult age group [17-19].
In the current study, our results suggested acceptable survival (5-year OS, 54.0%) in patients aged ≥ 70 years. Recently, a study by Sze et al. [9] found that the 5-year OS rate was 43.9% among patients aged ≥ 70 years. This inconsistency might be due to the application of IMRT in our study, which has shown to produce exceptional treatment results compared with 2DRT [20,21], but only 29.1% of patients in the study of Sze et al. [9] received IMRT. Additionally, considering the performance status of patients aged ≥ 70 years varying greatly, the heterogeneity of patients included in the study by Sze et al. [9] and the present study might contribute to the inconsistency of treatment outcomes. Results of our study demonstrated that ACE-27 was the strongest prognostic factor for OS in elderly patients aged ≥ 70 years. Considering that patients aged ≥ 70 years are commonly in close association with multiple comorbidities and poor performance status, which effect treatment outcomes, the use of ACE-27 score in the evaluation of elderly patients is necessary in the present study. In fact, the association between survival and ACE-27 has been demonstrated in a wide range of different cancers [22], and specifically in head and neck cancers [12,23]. Rogers et al. [23] evaluated the prognostic value of ACE-27 on head and neck cancer patients, and suggested that ACE-27 was robustly correlated with survival. Paleri et al. [24] even found that moderate and severe comorbidity evaluated using ACE-27 had a greater impact on survival than TNM stage in laryngeal squamous cancer patients. In contrast, Ramakrishnan et al. [25] reported that ACE-27 had no adverse role on 59 NPC patients’ prognosis. This inconsistency might be a result of small sample size, as noted by the authors.
Given the limited number of studies, the efficacy of chemotherapy in elderly patients with NPC remains unclear. Two prior studies [6,7] demonstrated that chemotherapy was associated with superior OS in elderly NPC patients after 2DRT. In contrast, our results failed to confirm the role of chemotherapy as a prognostic factor in elderly patients treated with IMRT. Considering that IMRT was adopted in the current study, this seems to be reasonable as patients had improved survival outcomes after IMRT [20,21], by which the actual benefit of chemotherapy might be diluted for this group. However, it should be mentioned that potential selection bias was hard to avoid in the use of chemotherapy in the present study. Further propensity-matched study or even randomized clinical trial are still needed to confirm the effect of chemotherapy in patients ages ≥ 70 years treated by IMRT.
In respect to previous studies, approximately 70% of NPC adult patients are diagnosed with stage III/IVA-B [16-18]. While we found higher proportion (83.3%) of patients with stage III/IVA-B in the current study, only two patients (1.6%) had stage I disease. Additionally, several studies [19,26] reported that among adult patients with NPC, approximately 40% presented with cervical mass. However, in the current study, cervical mass was present at diagnosis in 50% of patients. This suggests elderly patients who develop NPC may not have received prompt diagnosis and evaluation. Delayed diagnosis may occur in patients aged 70 years and older because of easily overlooked symptoms such as rhinobyon, headache, and tinnitus. Thus, for elderly patients, physicians should be more aggressive in the workup and diagnostic evaluation of NPC symptoms, as well as provide timely biopsies and nasopharyngoscope exams if indicated.
TLI is a serious late sequela following radical RT of NPC and associated with severe impairment of quality of life and survival [27]. Temporal lobe protection is arduous, particularly in patients with T3-4 disease that may have extensive skull base invasion or cavernous sinus involvement. Reported rates of TLI range from 7.5% to 12.9% in NPC patients after IMRT [28-30]. Given the high proportion of T3-4 disease (79%) in the current series, TLI incidence is expected to increase. However, in the present study, the incidence of 3.2% is lower than reported in prior studies. Moreover, given the poor survival among NPC patients older than 70 years [8,9], findings that they did not show a high incidence of TLI was probably due to a high proportion may have died prior to TLI could have develop. Therefore, the incidence of TLI in elderly patients may have been underestimated in the present study.
One major limitation in the present study is the small patient sample size and the influence this may have had on identifying an effect. However, the low NPC incidence in elderly patients must be noted, particularly those aged ≥ 70 years. Another limitation is that our study was limited by the retrospective nature, and the possible selection bias of using chemotherapy for patients was difficult to avoid. Additionally, a third concern was the lack on inclusion of data about pretreatment Epstein–Barr Virus DNA concentrations, which has shown to strongly predict NPC survival [31-33]. Further studies (e.g., propensity-matched study) are urgently needed to classify subgroups that would benefit most from chemotherapy, since not all patients aged ≥ 70 years can benefit from chemotherapy.
In summary, our results suggest that IMRT +/– chemotherapy has a manageable toxicity and provides an acceptable survival in patients aged ≥ 70 years. We observed a significant association between ACE-27 score with survival outcomes in this group of patients. Although we failed to confirm the benefit of chemotherapy for this group of patients, further studies are urgently needed to classify the subgroup who could gain most from chemotherapy.
Notes
Conflict of interest relevant to this article was not reported.
Acknowledgements
The present study was funded by the National Science & Technology Pillar Program during the Twelfth Five-year Plan Period (No.2014BAI09B10).