Breast Conservation Therapy Versus Mastectomy in Patients with T1-2N1 Triple-Negative Breast Cancer: Pooled Analysis of KROG 14-18 and 14-23
Article information
Abstract
Purpose
The aim of this study is to compare the treatment outcomes of breast conserving surgery (BCS) plus radiotherapy (RT) versus mastectomy for patients with pT1-2N1 triple-negative breast cancer (TNBC).
Materials and Methods
Using two multicenter retrospective studies on breast cancer, a pooled analysis was performed among 320 patients with pT1-2N1 TNBC. All patients who underwent BCS (n=212) receivedwhole breast RTwith orwithoutregional nodal RT,while nonewho underwent mastectomy (n=108)received it. All patients received taxane-based adjuvant chemotherapy. The median follow-up periods were 65 months in the BCS+RT group, and 74 months in the mastectomy group.
Results
The median age of all patients was 48 years (range, 24 to 70 years). Mastectomy group had more patients with multiple tumors (p < 0.001), no lymphovascular invasion (p=0.001), higher number of involved lymph node (p=0.028), and higher nodal ratio ≥ 0.2 (p=0.037). Other characteristics were not significantly different between the two groups. The 5-year locoregionalrecurrence-free, disease-free, and overall survivalrates of BCS+RT group versus mastectomy group were 94.6% versus 87.7%, 89.5% versus 80.4%, and 95.0% versus 87.8%, respectively, and the differences were statistically significant after adjusting for covariates (p=0.010, p=0.006, and p=0.005, respectively).
Conclusion
In pT1-2N1 TNBC, breast conservation therapy achieved better locoregional recurrencefree, disease-free, and overall survival rates compared with mastectomy.
Introduction
Triple-negative breast cancer (TNBC) has the higher risk for locoregional recurrence than any other molecular subtypes in the absence of effective targeted agents which are known to further decrease locoregional recurrence [1]. Therefore, there have been concerns on the potentially increased risk of locoregional recurrence after breast conservation therapy in TNBC [2-5]. Although a meta-analysis demonstrated the improved locoregional control by breast conserving surgery (BCS) plus radiotherapy (RT) compared with mastectomy alone in TNBC [6], stage-specific comparisons were not performed in this meta-analysis.
Recently, the survival benefit of breast conservation therapy over mastectomy alone in the early stage breast cancer has been suggested in the population-based studies [7-10], but molecular subtypes were not considered in these studies. Among patients with early stage breast cancer, pT1-2N1 has become the candidate for intensifying treatment, with the addition of regional nodal RT or post-mastectomy RT. In the absence of specific guidelines on post-mastectomy RT in pT1-2N1 breast cancer, it is still questionable whether mastectomy alone is a sufficient local treatment for pT1-2N1 TNBC.
In Korea, the number of breast cancer patients and those receiving RT for breast cancer is increasing [11]. Among them, the prevalence of TNBC was reported to be about 20%, and the surgical type did not impact on the 3-year survival in the registry data including 5,586 TNBC patients with various stages [12]. However, the receipt of RT was not analyzed as the covariate.
Given these observation, we compared the treatment outcomes of BCS+RT versus mastectomy alone for patients with pT1-2N1 TNBC via a pooled analysis of multicenter retrospective studies conducted by Korean Radiation Oncology Group (KROG).
Materials and Methods
1. Study population
Two multicenter retrospective studies on pN1 breast cancer were conducted by KROG: KROG 14-18 and 14-23. KROG 14-18 was designed to evaluate the role of regional nodal RT in addition to whole breast RT [13], and KROG 14-23 was to evaluate the recurrence outcomes after mastectomy without adjuvant RT [14]. Among patients enrolled in these two studies, 320 patients with pT1-2N1 TNBC were selected for a pooled analysis. Patients treated with BCS+RT were compared with those undergoing mastectomy alone in terms of patient and tumor characteristics as well as the treatment outcomes.
2. Treatment
All patients underwent upfront surgery, either BCS or mastectomy, with axillary lymph node dissection or sentinel lymph node biopsy. All patients who underwent BCS received adjuvant RT, while none who underwent mastectomy received it. Adjuvant RT was given to whole breast up to a median dose of 50.4 Gy (range, 45 to 50.4 Gy) with 1.8-2 Gy/fraction. The median dose of tumor bed boost was 9 Gy (range, 8 to 16 Gy). Regional nodal RT was determined at the discretion of attending radiation oncologists. As for systemic therapy, all patients received taxane-based adjuvant chemotherapy.
3. Statistical analysis
Locoregional recurrence-free survival (LRRFS), diseasefree survival (DFS), and overall survival (OS) rates were estimated from the date of surgery by Kaplan-Meier method. To evaluate risk factors associated with each endpoint, logrank test was used for univariate analysis. For multivariate analysis, Cox proportional-hazards model was used incorporating factors seemed to be significant on univariate analysis (p < 0.2). Otherwise, a p-value of < 0.05 was considered statistically significant. A chi-square test was used for comparison among categorical variables. All analyses were performed in PAWS Statistics for Windows, ver. 18.0 (SPSS Inc., Chicago, IL).
4. Ethical statement
The institutional review board approved these studies (approval number: SMC 2014-12-005 at Samsung Medical Center for KROG 14-18 and H-1503-053-655 at Seoul National University Hospital for KROG 14-23), and waived the requirement for obtaining informed consent.
Results
1. Characteristics
The median age of all patients was 48 years (range, 24 to 70 years). Most patients had invasive ductal carcinoma (96.6%). One hundred and six patients (33.1%) had T1 tumors, and 214 patients (66.9%) had T2 tumors. The number of involved lymph node (LN) was one in 187 patients (58.4%), two in 82 (25.6%), and three in 51 (15.9%). The nodal ratio was ≥ 0.2 in 48 patients (15.0%).
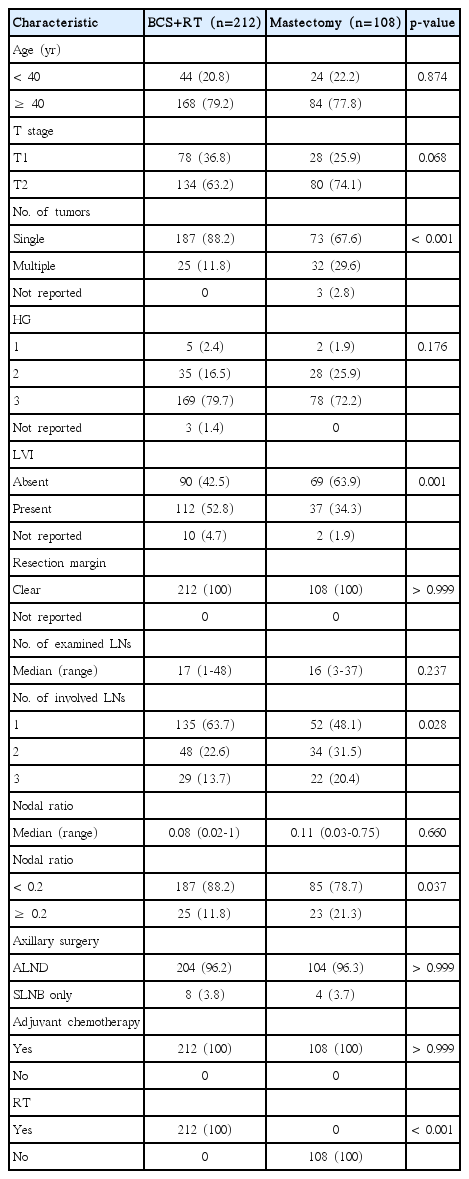
Patient and tumor characteristics according to the treatment were summarized in Table 1. Mastectomy group had more patients with multiple tumors (p < 0.001), no lymphovascular invasion (LVI) (p=0.001), higher number of involved LN (p=0.028), and higher nodal ratio (p=0.037). Other characteristics were not significantly different between the two groups.
In the BCS+RT group, whole breast RT alone was given to 141 patients (66.5%), whole breast plus supraclavicular nodal RT to 59 (27.8%), and whole breast plus supraclavicular/internal mammary nodal RT to 12 (5.7%). As for systemic chemotherapy, 304 patients (95.0%) received anthracyclinebased chemotherapy followed by taxane, 14 patients (4.4%) received taxane-anthracycline combination chemotherapy, and two patients (0.6%) received taxane plus cyclophosphamide.
2. Patterns of failure
The median follow-up period was 65 months in the BCS+RT group, and 74 months in the mastectomy group. As the cumulative events, there were 11 local recurrences; six in BCS+RT group and five in mastectomy group. Regional recurrences occurred in 18 patients; seven in BCS+RT group and 11 in mastectomy group. Distant metastases were present in 41 patients; 20 in BCS+RT group and 21 in mastectomy group.
3. Survival outcomes and prognostic factors
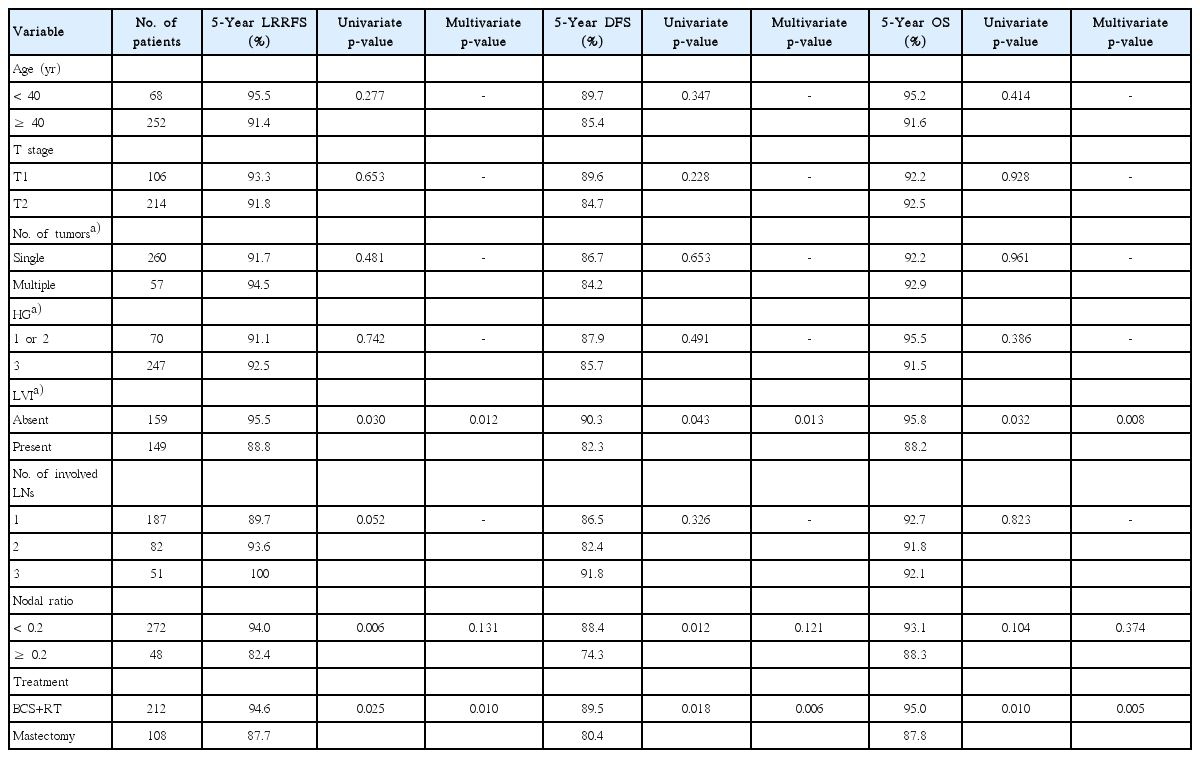
The univariate and multivariate analyses for LRRFS, DFS, and OS were presented in Table 2. The 5-year LRRFS rate was 94.6% in BCS+RT group and 87.7% in mastectomy group (p=0.025). Presence of LVI (p=0.030) and nodal ratio ≥ 0.2 (p=0.006) were also significantly associated with inferior LRFFS on univariate analysis. After adjusting treatment group, LVI, and nodal ratio, BCS+RT as well as the absence of LVI achieved a superior LRRFS (p=0.010 and p=0.012, respectively) (Fig. 1A).
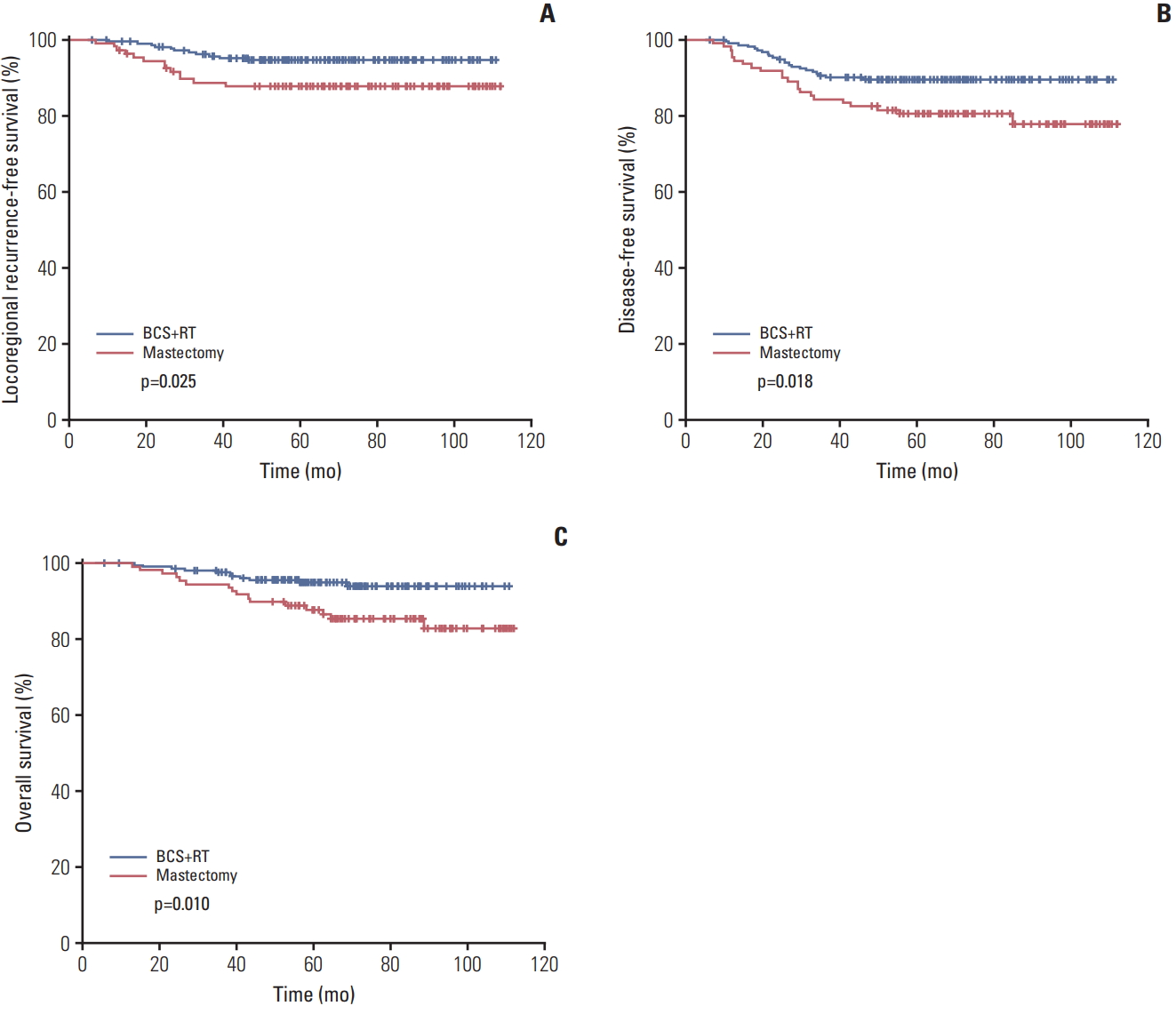
Locoregional recurrence-free survival (A), disease-free survival (B), and overall survival (C) curves according to the treatment. BCS, breast conserving surgery; RT, radiotherapy.
When the LRRFS was separated into local recurrence-free and regional recurrence-free survival rates, BCS+RT group showed a better regional recurrence-free survival rate than mastectomy group (5-year rate, 96.6% vs. 89.6%, respectively; p=0.011), but the local recurrence-free survival rates were similar (5-year rate, 97.1% vs. 95.3%, respectively; p=0.404).
In addition, BCS+RT resulted in a superior DFS compared with mastectomy (89.5% vs. 80.4% at 5 years, p=0.018) (Fig. 1B). As for OS, BCS+RT was also correlated with a better outcome (95.0% vs. 87.8%, p=0.010) (Fig. 1C). After adjusting treatment group, LVI, and nodal ratio, BCS+RT and the absence of LVI were favorable prognosticators for both DFS (p=0.006 and p=0.013, respectively) and OS (p=0.005 and p=0.008, respectively).
Discussion
TNBC is a well-known entity of aggressive clinical behavior and poor prognosis [1]. While breast conservation therapy has been established as the appropriate local therapy for most of early stage breast cancer [15,16], mastectomy is still performed in a significant number of patients. Moreover, considering a higher rate of locoregional recurrence in TNBC, the optimal local therapy for these patients has been under debate [2-5]. Regarding this issue, a meta-analysis by Wang et al. demonstrated that BCS+RT was less likely to develop locoregional recurrence compared with mastectomy, but comparisons according to specific stage were not performed [6]. More recently, Abdulkarim et al. [17] showed that BCS+RT resulted in a better locoregional control compared with mastectomy in pT1-2N0 TNBC, while a comparable locoregional control between the two groups was shown in a similar population from Memorial Sloan Kettering [18].
Other investigators also analyzed the impact of adjuvant RT among TNBC patients with various stages, and the results were inconsistent. Kindts et al. [19] reported that BCS+RT showed a higher breast cancer-specific survival in the whole population compared with mastectomy alone, but not in pT1-2N0 subgroup. Similarly, multi-institutional analysis from five Asian cancer centers demonstrated that BCS+RT was associated with a superior OS compared with mastectomy alone in the whole population, but not in pT1-2N0-1 subgroup [20]. However, there are few studies analyzing the specific subgroup of pN1 TNBC. In the aforementioned studies, moreover, the number of patients with pN1 disease in the BCS+RT or mastectomy groups was only 59 and 141, respectively.
In the present study, only patients with pT1-2N1 TNBC were analyzed, and the number of patients in the BCS+RT and mastectomy groups was 212 and 108, respectively. In addition, all patients completed taxane-based adjuvant chemotherapy, and 95% of patients received anthracyclinebased chemotherapy followed by taxane. Without effective targeted agents such as endocrine therapy or anti-HER2 therapy, chemotherapy is the mainstay of systemic treatment for TNBC. Appropriate usage of chemotherapy is well known to be associated with better local control as well as survival outcomes [21]. With the sufficient number of patients treated with appropriate systemic therapy, our study showed that BCS+RT improved LRRFS, DFS, and OS compared with mastectomy alone in pT1-2N1 TNBC. This observation also suggests that definitive local modality cannot be completely replaced with taxane-based chemotherapy in TNBC and post-mastectomy RT should be considered for these patients.
In the historical randomized trials conducted in the 1980s, BCS+RT and mastectomy achieved an equivalent OS in the early stage breast cancer [15,16]. However, in the real-world situation, there are several reports observing the superiority of breast conservation therapy over mastectomy [7-9]. Regarding this discrepancy, the selection bias cannot be fully excluded, but the improvement of radiotherapeutic technique and systemic therapy might also contribute to these results. It is well known that with the increased systemic control with newer chemotherapeutic regimens, local control could be translated into OS benefit [22]. A recent populationbased study from Netherlands also noted that BCS+RT significantly improved long-term survival of pT1-2N0-1 breast cancer compared with mastectomy, and such improvement was consistently observed in all T and N categories [10]. However, the impact of molecular subtypes was not fully considered in these studies, but only information on hormonal receptor status was collected. The present study supports the conclusion of these population-based studies in patients with pT1-2N1 TNBC, whom the risk of recurrences is higher and the benefit of RT might be prominent than in those with more indolent diseases.
Considering 12.3% of patients experienced locoregional recurrence after mastectomy at 5 years in the current study, post-mastectomy RT needs be considered for these patients. Recent guideline update from American Society of Clinical Oncology, American Society for Radiation Oncology, and Society of Surgical Oncology also noted that post-mastectomy RT reduces the risks of locoregional recurrence in pT1-2N1 breast cancer, but many other clinicopathologic factors should be considered together in the decision making [23]. Although many investigators sought to find out such indications for pT1-2N1 breast cancer [24-26], however, the role and/or indication of post-mastectomy RT is beyond the scope of our study.
Given the positive results of recent randomized trials [27,28], the role of regional nodal RT becomes more important in the treatment of early stage breast cancer. According to the Canadian trial, the survival benefit was prominent especially in hormonal receptor-negative tumors [27]. In our study, about one-third of patients received regional nodal RT, but supraclavicular/internal mammary nodal RT was given to only 5.7% of patients. Despite this, the improved LRRFS of BCS+RT group comes mainly from better regional control. One possible explanation is that a significant portion of axilla was included in the whole breast RT field [29]. When the regional recurrences were divided into subsites, eight of 11 regional recurrences were of axilla in the mastectomy group, whereas two of seven in the BCS+RT group (data not shown). More comprehensive nodal RT might further improve the outcomes of TNBC patients with nodal involvement.
This study has the typical shortcomings from the retrospective nature of the study design. Some characteristics between the two groups were different, and selection biases might not be fully resolved via multivariate analysis. In addition, the follow-up period was relatively short, although most recurrences of TNBC are known to occur within 2-3 years.
In conclusion, breast conservation therapy achieved better LRRFS, DFS, and OS rates compared with mastectomy alone in patients with pT1-2N1 TNBC. The role of post-mastectomy RT should be evaluated for these patients.
Notes
Conflict of interest relevant to this article was not reported.