Modest Anti-Cancer Activity of a Bile Acid Acylated Heparin Derivative in a PC14PE6 Induced Orthotopic Lung Cancer Model
Article information
Abstract
Purpose
A novel chemically modified heparin derivative, heparin-deoxycholic acid nano-particles, has lower anticoagulant activity, and was recently reported to have significant anti-tumor effects on squamous head and neck cancer cells. Therefore, the aim of this study was to evaluate the anti-tumor effects of heparin-deoxycholic acid nano-particles in a human lung adenocarcinoma cell line.
Materials and Methods
An orthotopic lung cancer model in 16 mice was developed using intra-thoracic injections of 0.5×106 PC14PE6 cells. Ten days after inoculation, the mice were divided into two groups. PBS and Heparin-DOCA particles were injected once a day every 3 days in the tail vein, for a total of 5 injections. The body weight and survival of each mouse were monitored and the tumor size in the lung was measured by SPECT-CT before and after heparin-DOCA nano-particle treatment.
Results
IThe HD particles had no significant cytotoxicity when the PC9 cells were treated in vitro. There was no statistical difference in tumor size, body weight and survival between the HD treated and control groups in vivo. Furthermore, there was no difference in the amount of CD31 between tumor tissues in the two study groups.
Conclusion
HD synthesized with unfractionated heparin had no apparent inhibitory effects on tumor growth in a PC14PE6 cell induced orthotopic lung cancer mouse model. The HD particles did not significantly inhibit tumor-induced angiogenesis at the tumor sites.
Introduction
Non-small cell lung cancer (NSCLC) is one of the most common malignancies globally and is the leading cause of cancer-related death worldwide and in Korea (1,2). In spite of recent therapeutic advances, the treatment outcome for advanced NSCLC remains disappointing: the five year survival rate has steadily remained around 15% (3-5). Although platinum-based doublet chemotherapy has been the standard treatment for advanced NSCLC, the survival benefits have been frequently offset by substantial toxicity. Therefore, novel anti-cancer therapies should focus on the trade-off between treatment efficacy and toxicity while attempting to improve the quality of life.
Various independent studies, using different cancer models, have shown that unfractionated and low-molecular-weight heparin significantly inhibits spontaneous metastasis by directly blocking selectins (6-10). Heparin is a highly sulfated natural polysaccharide that is mainly composed of alternating units of sulfated glucuronic acid and glucosamine derivatives. As a result of its interference with bFGF and VEGF activity, heparin has been shown to inhibit angiogenesis and tumor metastases in several studies (7,11). Despite the apparent anti-cancer effects, the long-term administration of high dose heparin is significantly limited due to the associated hemorrhagic complications.
In an attempt to increase clinical applicability, heparin derivatives with lower anticoagulant activity have been developed, and evaluated for their inhibitory effects on angiogenesis, tumor growth, and metastasis (10,12,13). A novel chemically modified heparin derivative, heparin-DOCA (HD) particles, was recently reported to have significant anti-tumor effects in squamous head and neck cancer cells (14). This heparin derivative has low anticoagulant activity that may facilitate the use of higher heparin doses with fewer hemorrhagic side effects. In addition, given that HD has a strong negative charge and a hydrophobic segment, HD may be used as a drug carrier. HD particles have been reported to inhibit tumor-induced angiogenesis by suppressing the phosphorylation of FGFR and its downstream signal pathways (ERK and p38 MAPK activities) (14). Treatment with heparin may inhibit or stimulate tumor growth and metastasis depending on the cancer cell type and the animal model studied (6). Thus, the effects of HD require further investigation in a variety of human cancer cell lines to determine its anti-cancer activity. In the current study, we evaluated the anti-tumor effects of HD particles in a human lung adenocarcinoma cell line and an orthotopic mouse model.
Materials And Methods
1 Animals and animal care
Male BALB/c nude mice weighing 20~25 g (Orient, Korea), were maintained at 25℃ on a standard diet and restricted water for at least 1 week before the experiments in pathogen-free conditions. All animals received human care in compliance with the "Guide for the Care and Use of Laboratory Animals" prepared by the institute of laboratory animal resources and published by the National Institutes of Health and The Animal Experiment Guided lines of Samsung Biomedical Research Institute.
2 Orthotopic lung cancer models
An orthotopic lung cancer xenograft animal model was developed as previously described (15). Briefly, the mice were anesthetized with an intra-peritoneal injection of an aqueous solution (5 ml/kg) of xylazine (8 mg/kg) and ketamine (120 mg/kg). Then 0.5×106 of human lung adenocarcinoma PC14PE6 cell suspension, with growth factor-reduced Matrigel (Becton Dickinson & Co., San Jose, CA), was inoculated directly into the left lung of the mice by intra-thoracic injection. The animals were observed for 30 min until full recovery from the anesthesia. The body weight of the animals was recorded every two days after the tumor inoculation.
3 Heparin-DOCA particle preparation
Lyophilized heparin-deoxycholic acid (HD) particles were kindly provided by Professor Byun from the Laboratory of Cell and Macromolecule Delivery, College of Pharmacy, Seoul National University, Seoul, Korea. Briefly, the heparin-DOCA was synthesized by reacting heparin with the bile acid analogue, N-deoxycholylethylenediamine (DOCA-NH2), as previously described (16). Heparin (0.1 g) was dissolved in formamide (5 mL) by gentle heating. EDAC (0.096 g) was mixed with this heparin solution, and this was followed by DOCA-NH2 (1.086 g) dissolved in anhydrous DMF (5 mL). Dried heparin-DOCA was suspended in water and lyophilized to produce white powder. For the I.V. injections, the HD particles were dissolved in PBS at a 1 mg/mL concentration and sterilized using a 0.45 µm pore size syringe filter. The size of the HD particles was measured by a DLS instrument (Zetasizer, Nano-ZS, Malvern Instruments Ltd., UK).
4 Cytotoxicity
The PC9 cells, a human lung adenocarcinoma cell line, were maintained in RPMI1640 (Gibco, Canada) supplemented with 10% heat-inactivated fetal bovine serum and penicillin streptomycin. Cells were cultured in a humidified atmosphere of 5% CO2 in air in a 37℃ incubator. To investigate the cytotoxicity of the HD particles, the PC9 cells were cultured in 96 well plates at 5,000 cells per well, one day before the experiment. The HD particles and heparin (H0777, Sigma, North York, Ontario) were added in a 1/5 serial dilution starting with a beginning concentration of 100 µg/mL After 72 h of incubation, the cells were assessed by a viability assay using the Cell Counting Kit-8 (CCK-8, Dojindo, Japan) according to the manufacturer's manual.
5 SPECT-CT imaging
SPECT-CT images were used to observe real-time tumor development in the lungs. In addition, the tumor size was monitored using a protocol developed at the Department of Nuclear Medicine, Samsung Medical Center, as previously reported (17). Serial CT imaging data was acquired using a SPECT-CT scanner while the animal was anesthetized after intra-peritoneal injection of an aqueous solution (5 mL/kg) of xylazine (8 mg/kg) and ketamine (120 mg/kg).
Once the lung tumor nodules were detected by SPECT-CT, the 16 mice were divided into two groups. The experimental group received intravenous (I.V.) injections of 0.2 mL of HD particles in PBS (10 mg/kg) every 3 days, for a total of five injections as described previously (14). The control group received PBS only. Following intravenous administration, we obtained serial CT images at six days and 13 days after inoculation. The 3-Dimensional whole length (x=a, y=b, z=c) of the tumor was recorded from the SPECT-CT images and the tumor volume was calculated according to the formula V=πabc/6. All animals were autopsied after they were euthanized and histological examinations were performed.
The length of the transverse plane (a) was marked with an x, and indicated the length of the tumor mass from the left to the right side; the length of the coronal plane (b) was marked by a y, and indicated the length of the tumor mass in the up and down direction; the length of the sagittal plane (c) was marked by a z, and indicated the length of the tumor mass from front to back. These three lengths a, b, and c were added to the formula for an ellipsoid V=4πr1r2r3/3 (r1 is the semidiameter of length of the ellipsoid; r2 is the semidiameter of width of the ellipsoid; r3 is the semidiameter of height of the ellipsoid), and converted into V=πabc/6. The volume of all of the tumor masses, from the animals in this experiment, was calculated with the converted formula described above according to the, a, b, c size measurements from the SPECT-CT images (Fig. 2).

SPECT-CT images of orthotopic lung cancer. 3 Dimensional images were generated by SPECT-CT scanning. The length of the transverse plane=a was marked as x, and indicated the length of the tumor mass from the left to right side; the length of the coronal plane=b was marked as y, and indicated the length of the tumor mass up and down; the length of the sagittal plane=c was marked as z, and indicated the length of the tumor mass from front to back. The volume of the tumor in the mouse lung was calculated according to the formula V=πabc/6.
6 Immunohistochemistry
To evaluate angiogenesis identified in the tumor mass, the whole lung including the tumor was removed from the controls and the HD particle treated animals for evaluation. The tissues were fixed in 10% neutral formalin and embedded in paraffin. The paraffin-embedded tissues were sectioned into 5 µm thick slices and dewaxed in xylene, re-hydrated with descending concentrations of ethanol and immunostained with the CD31 antibody, a blood vessel marker (SC-101454, Santa Cruz, CA). After primary antibody treatment, the sections were treated with rabbit anti rat IgG and developed with the Real EnVision Detection System (K5007, DAKO, Denmark), followed by Mayer's hematoxylin counter-staining. The number of CD31-positive blood vessels in five high power fields (×200) in the tumor sections from the controls and the HD particle treated animals were counted and averaged.
7 Statistics
The statistical significance of the differences between the experimental and control groups were determined using the student t test. p-values were considered significant when at a p<0.05. This study was approved by the Institutional Animal Care and Use Committee (IACUC) of Samsung Biomedical Research Institute (SBRI). The SBRI is an Association for Assessment and Accreditation of Laboratory Animal Care International (AAALAC International) accredited facility and abides by the Institute of Laboratory Animal Resources (ILAR) guide.
Results
1 Characterization of HD particles
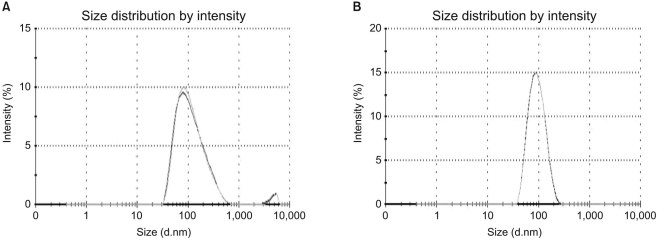
Fig. 1 shows the size of the HD particles dissolved in the PBS. Although the HD particles are highly soluble in lyophilized powder, the results of the Zeta-sizer indicated that there were some aggregates (a). The solution, after filtration with a 0.45 µm pore size syringe filter, demonstrated a uniform size distribution of about 89±2.2 nm (b), which was smaller than the previously described size of 120±2.9 nm (18). The pH of the HD particle solution was measured as ~7.0, which was similar to the physiological pH.
2 The orthotopic lung cancer model and cell viability assay
An orthotopic lung cancer model was established using PC14PE6 cells in nude mice. As illustrated in Fig. 2, a tumor mass was generated in the lungs of the mice approximately 10 days after direct thoracic injection of 0.5×106 of the PC14PE6 cells. The tumor mass was confirmed by SPECT-CT imaging and the volume of the tumors was measured. The success rate of establishing the orthotopic model using the PC14PE4 cells was 100% (16/16), and the mean diameter of the longest axis was 4.59±0.355 mm.
There was no significant difference in cell cytotoxicity when the lung cancer cells were treated with HD particles in vitro (Fig. 3). In addition, there was no difference in body weight between the treated and control groups (Fig. 4A).
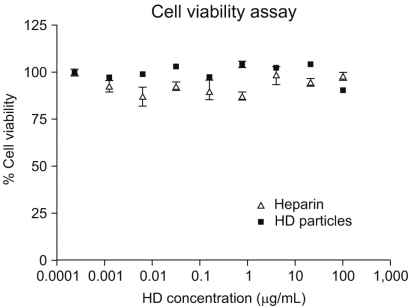
Cytotoxicity of HD particles. Cell viability assay of HD particles compared with the same dose of heparin in the PC9 cells. There was no significant difference between the heparin and HD particle treated groups. (△) Heparin treated group (■) HD particle treated group.
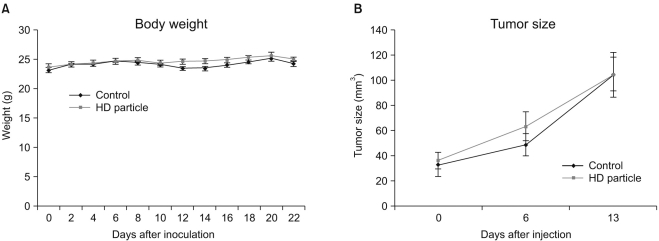
Effects of HD particles on body weight and tumor volume. The mean body weight of the two groups was not significantly changed during the study; the control and HD treated groups were not significantly different (A). The mean size of the tumor volume at three intervals in the HD particle treated group was similar to the control group (B); the difference between the groups was not statistically significant (p>0.05).
3 Anti-tumor activity of HD particles
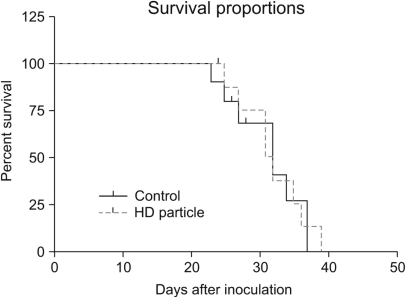
Tumor size in the mouse lungs was first measured by SPECT-CT 10 days after cancer cell inoculation. The HD particles were administered via tail vein injection after confirmation of tumor growth by SPECT-CT. The HD particles were given at 0, 3, 6, 9, and 12 days after the tumor was visualized in the mouse lung by SPECT-CT, at three intervals. As shown in Fig. 4B, when treatment was started, the mean size of the tumors (at post-inoculation day 10) was 36.18±6.44 mm3 in the HD treated group and 33.03±9.50 mm3 in the control group. At the second interval, the mean size of the tumors at post-treatment day 6 was 62.95±11.47 mm3 for the HD treated group and 48.03±8.71 mm3 for the control group. The last time, at post-treatment day 13, the mean size of the tumors was 104.22±17.90 mm3 in the HD treated group and 104.19±13.44 mm3 in the control group. There was no statistical difference in tumor growth between the HD treated group and the control group. When the size of the tumors was expressed as a proportion of the initial tumor volume, in order to estimate the rate of tumor growth, there was only a trend toward tumor growth inhibition at post-treatment day 13 (data was not shown); however, this was not statistically significant (p>0.05). Furthermore, there was no statistical difference in survival between the HD particle treated and the control groups (mean survival duration; treated vs. control; 29.9±1.9 vs. 31.0±1.6 days, respectively; Fig. 5) (p=0.943).
4 Anti-angiogenic effects of HD on the lung cancer cells
The average numbers of CD31-positive blood vessels in five high power fields (×200) among the tumor sections from the PBS treated animals and HD particle treated animals were 35.83±2.15 and 34.83±2.50, respectively. The HD particles did not significantly inhibit tumor-induced angiogenesis in the lung cancer model (Fig. 6).
Discussion
In this study, we investigated the antitumor effects of heparin-DOCA particles in non-small cell lung cancer cells via inhibition of angiogenesis; such effects have been previously demonstrated in other cell types including head and neck cancer cells in vitro (14). It has been reported that heparin derivatives may exert stimulatory or inhibitory effects against cancer cells depending on the cancer cell type. In contrast to its anti-cancer effect on head and neck squamous cells, HD particles did not exert any significant effect on the PC14PE6 cells, which are human lung adenocarcinoma cells. HD particles did not inhibit angiogenesis or tumor growth in our model. There was a trend towards tumor growth inhibition by post-treatment day 13 (HD treated vs. control; 2.93±0.20% vs. 4.02±0.85%, respectively), although these differences were not statistically significant (p>.05). In addition, there appeared to be a minimal survival gain rendered by HD particle treatment in the lung adenocarcinoma animal model (mean survival duration; HD treated vs. control; 31.0±1.6 vs. 29.9±1.9 days, respectively; Fig. 5) (p=0.943).
There is an increasing body of evidence that heparins inhibit tumor metastasis and progression (6,8,9). Furthermore, the results of several prospective clinical trials have suggested that this anticoagulant may interfere with cancer progression and may provide a survival benefit, especially in patients with a better life expectancy (7,11,19). Heparin is thought to exert its anti-tumor effects mainly via inhibition of P-selectins and L-selectins during the initial survival stage of tumor cells in the circulation (8,20,21). However, the use of native heparin as an anti-cancer agent is limited due to its potent anticoagulant activity and frequent dosing schedule required to achieve appropriate therapeutic levels. Therefore, a chemically modified heparin derivative with similar anti-cancer activity that has lower anticoagulant effects might provide a useful form of therapy in the clinical setting.
The chemically modified heparin derivative, HD particles, has been reported to inhibit the formation of capillary-like vascular structures, slows vascularization within Matrigel plugs implanted into mice, and prevents the proliferation of endothelial cells, in head and neck tumor cells, thereby suppressing angiogenesis and tumor growth (14). Moreover, HD particles have been shown to inhibit intercellular interactions between B16F10 melanoma cells and activated platelets by blocking P- and E-selectin-dependent interactions, and reduced adhesion and migration of tumor cells to the extracellular matrix, thereby preventing tumor cell retention in the lungs (22). Heparin-DOCA attenuated lung colony formation on the surface and in the interior of the lungs, and attenuated metastasis by B14F19 melanoma cells and SCC7 head and neck cancer cells (22). Although many studies have reported on the anti-metastatic effects of heparins, in several tumors, by interfering with the cells on the endothelial wall of blood vessels, only a few studies have evaluated the effects of heparin, or its derivatives, on the proliferation of cancer cells and, the results of these studies are inconclusive and depend on the type of heparin or derivatives used (6).
Based on the promising anti-tumor activity observed in melanoma and head and neck cancer cells, we tested the anti-tumor effects of heparin-DOCA derivatives synthesized with unfractionated heparin in human lung adenocarcinoma cells in vitro and in vivo using an orthotopic animal model. Although the data are not shown, we tested its efficacy in other lung cancer cell lines including PC9, HCC827 and A549 cells to exclude a specific cell line effect; there were no direct anti-tumor effects in these cell lines either. Unlike the suppression effects of heparin on metastasis of tumor cells, by interfering with cell to cell adhesion by blocking selectins, its effects on the inhibition of tumor growth in vivo have been reported to be associated with anti-angiogenic activity (14,23). However, we did not observe a statistically significant difference in the rate of tumor growth and the number of blood vessels in the HD treated group compared to the PBS treated group in this study. Hence, there appears to be different anti-angiogenic activity associated with heparin-DOCA among different tumor types, with the underlying mechanisms not yet determined (24).
Prior studies of the inhibitory effects of heparin on angiogenesis at tumor sites have shown that LMWH, in contrast to UFH, can hinder the binding of growth factors to their receptors as a result of its smaller size and therefore enhanced specificity (25). Hence, synthesizing heparin derivatives from LMWH, not UFH, might be more potent in the inhibition of tumor growth. Now, we plan to investigate carefully whether these LMWH derivatives inhibit tumor growth through their anti-angiogenic effects in an orthotopic lung cancer model similar to the one described above.
Conclusion
HD particles (UFH-DOCA) did not have significant anti-cancer activity in a human adenocarcinoma lung cancer cell (PC14PE6) line and in an orthotopic lung cancer mouse model. Further study is planned to evaluate different heparin derivatives and doses.
Notes
This study was supported by a grant of the Korea Health 21 R&D Project Ministry of Health & Welfare, Republic of Korea (No. A050742).