Mixed Testicular Germ Cell Tumor Presenting as Metastatic Pure Choriocarcinoma Involving Multiple Lung Metastases That Was Effectively Treated with High-dose Chemotherapy
Article information
Abstract
Choriocarcinoma in the testis is very rare, and it represents less than 1% (0.3%) of all the testicular germ cell tumors. It is a particularly aggressive variant of non-seminoma tumor, which is characterized by a high serum β-HCG level and multiple lung metastases. The optimal management for this disease remains undefined. We report here on a case of choriocarcinoma with multiple lung metastases, and the patient has achieved continuous remission for 2 years after combination chemotherapy of BEP (bleomycin, etoposide and cisplatin) and sequential high-dose chemotherapy with autologous peripheral stem cell rescue.
Introduction
Choriocarcinoma is a highly malignant uncommon tumor of the testis, and it usually occurs as a component of mixed germ cell tumor (1). The testicular enlargement may be subtle, and the patient may present with multiple metastasis. Early metastases are usually found in most of these patients, and they most commonly occur in the lung, liver and brain. There is often marked elevation of the serum levels of human chorionic gonadotropin (hCG) (2). On gross examination, choriocarcinomas of the testis are often small and the involved testes may appear normal.
Metastasis from a testicular mixed germ cell tumor as pure choriocarcinoma is also uncommon (3). We report here on one case of metastatic pure choriocarcinoma with aggressive lymph node metastases and multiple pulmonary metastases, and the patient achieved complete remission after high-dose chemotherapy with autologous stem cell transplantation.
Case Report
A 33-year-old previously healthy man was referred to Soonchunhyang University Hospital, Korea in December 2006. He complained of abdominal pain, and numerous pulmonary nodules in both lungs had previously been incidentally detected. The patient had a one-month history of progressive abdominal pain and weight loss of 7 kg. No other signs and symptoms had been noted except for dyspepsia and questionable chest tightness. The patient had an acutely ill-looking appearance, and the physical examination of the other systems was unremarkable. His external genitalia were not examined at the first visit. The laboratory findings showed an elevated level of lactate dehydrogenase (LDH) of 1,156 U/L (reference range: 100~450 U/L) and an elevated level of β-HCG of 174,156.56 mIU/mL (reference range: 0~5 mIU/mL). The initial tests for the WBC, hemoglobin and alpha-fetoprotein (AFP) were 10,000/µL (reference: 4,000~10,000/µL), 13.3 g/dL (reference: 13~17 g/dL) and 0.99 ng/mL (reference: 0~6.0 ng/mL), respectively. The other laboratory findings were unremarkable. On an additional physical examination, the scrotum was grossly normal, but scrotal ultrasonography revealed a heterogenous and somewhat calcified mass in the right testis. An enhanced abdomino-pelvic and chest computerized tomogram (CT) showed multiple enlarged and conglomerated lymph nodes with central necrosis in the para-aortic, aorto-caval, retrocaval and mediastinal areas (Fig. 1, 2). We performed a right radical orchiectomy and one pulmonary nodule was resected via video-assisted thoracoscopic surgery (VATS). The pathologic findings of the testis and the pulmonary nodule were quite different. The right testicular mass was 1.3×1 cm and it was composed of mature teratoma without syncytiotrophoblastic and cytotrophoblastic tumor cells (Fig. 3). But the histologic findings of the right pulmonary nodule showed the background of extensive hemorrhage and necrosis, and small areas with multinucleated syncytiotrophoblasts and cytotrophoblasts (Fig. 4). On immunohistochemistry (IHC) staining, the tumor cells were positive for hCG and negative for alpha fetoprotein (AFP). We diagnosed the man as suffering with a mixed testicular germ cell tumor with lung metastasis that was composed of pure choriocarcinoma.
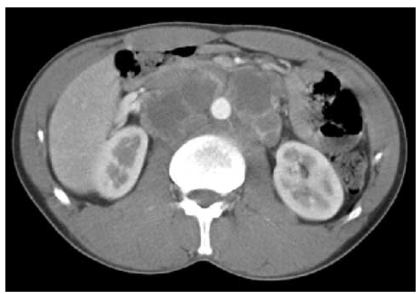
The abdominopelvic CT shows multiple enlarged and conglomerated lymph nodes with central necrosis in the paraaortic, aortocaval and retrocaval areas.

Chest CT shows multiple enlarged lymph nodes with central necrosis in the subcarinal area and hematogenous pulmonary nodules in both lungs.
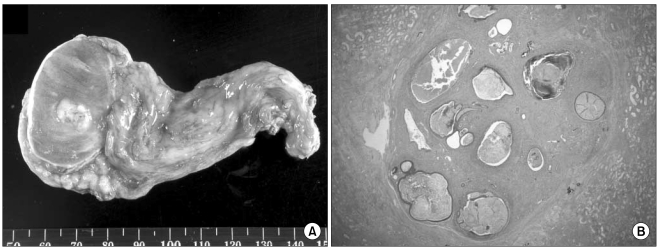
The right testis gross appearance (A) and H-E staining (×40), (B) revealed mature teratoma without dermoid and epidrmoid cysts.
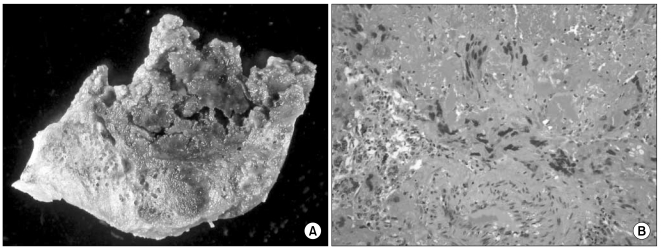
The gross appearance of the wedge-resected lung (A) and the H-E stain (×200), (B) revealed the presence of multinucleated syncytiotrophoblastic cells and extensive hemorrhagic necrosis.
The chest X-ray showed rapid aggravation of multiple lung metastases (Fig. 5) and the patient's condition had rapidly deteriorated during the 2 weeks prior to the confirming the diagnosis.
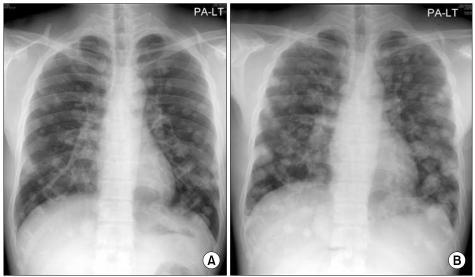
The initial chest PA (A) and the chest PA taken on the 15th day after admission (B). Variable sized round multiple nodules are noted in both lung fields. The chest X-rays show rapid progression of multiple lung metastases between (A) and (B).
The patient received four cycles of combination chemotherapy with bleomycin, etoposide and cisplatin (BEP). After combination chemotherapy, the LDH and β-hCG levels markedly decreased to 243 U/L and 13.71 mIU/mL, respectively (reference range for β-hCG: 0~5 mIU/mL), but the β-hCG had not reached the normal range. The abdomino-pelvic and chest CT demonstrated markedly reduced sizes of the retroperitoneal lymph nodes and the pulmonary nodules. However, as he had still numerous pulmonary nodules, retroperitoneal lymphadenopathy and an elevated β-hCG level, high-dose chemotherapy together with autologous stem cell transplantation was performed on June 2007. The peripheral blood stem cells (PBSCs) were collected by cyclophosphamide-mobilization before beginning high-dose chemotherapy. The high-dose chemotherapy regimen consisted of ifosfamide 2,500 mg/m2, carboplatin 500 mg/m2 and etoposide 600 mg/m2; this was intravenously given for 3 consecutive days (9,10). He is alive and has been continuously disease-free until June 2009.
Discussion
Non-seminomatous germ cell tumors are highly aggressive malignancies of the testis. Histologically, approximately 70% of the non-seminomatous germ cell tumors are composed of more than one germ cell component (mixed germ cell tumor), and this requires obtaining an appropriate specimen for making the correct diagnosis together with the correlation of the serum tumor markers (4,5). Choriocarcinoma is relatively rare among the various components of non-seminomatous germ cell tumors, including embryonal carcinoma, seminoma, yolk sac tumor and teratoma. Less than 8% of the testicular germ cell tumors contain a choriocarcinoma component, and pure choriocarcinoma accounts for only 0.3% of all the primary testicular germ cell tumors (6).
The term choriocarcinoma is generally used to refer to gestational choriocarcinoma, which most commonly occurs with hidatidiform mole, spontaneous abortion, ectopic pregnancy or normal delivery. It is a cancer that typically occurs in the chorionic epithelium of the placenta of females and it rarely occurs in males. Choriocarcinoma in the testis has a particularly high-risk histology and the patients with this tumor are prone to present with metastases rather than a testicular mass. The most common presenting symptoms include hemoptysis secondary to pulmonary metastases, back pain secondary to retroperitoneal spread, gastrointestinal bleeding due to gastrointestinal tract metastases and neurological symptoms that are due to brain metastases (7).
Yokoi K et al. recently reported on a review of the literature on choriocarcinoma (5). They examined the characteristics of this tumor based on 106 cases of male choriocarcinoma that were reported during the previous 12 years (1995 to 2005). The testis was the most common primary site at 33% (35/106), followed by the mediastinum, pineal body, gastrointestinal tract, lung and retroperitoneum. Metastasis was seen in 83% of the patients, with multiple metastases seen in most of the patients. The most common metastatic sites were the lung, liver and brain. The mean age of the males with choriocarcinoma was 36.0 years, and this tumor tended to occur in children and adolescent, where the age of two thirds of all the cases (69/106) was less than 30-years old. The prognosis of male choriocarcinoma was very poor, with the cumulative survival rate being 30%, and the course of the disease was rapid with the mean survival time being 7.7 months; 23.8% and 45.4% of the patients showed 1-month and 6-month mortality, respectively (5).
Our case presented with unique characteristics. The primary mass was teratoma without a choriocarcinoma component; the metastatic pulmonary nodule was pure choriocarcinoma. The metastases usually reflect the histology of the primary tumor. However, different histologic cell types are found more often in metastases than the same cell type of the primary tumors. This may be due to the maturation of the primary germ cell type into another cell type, or it may be due to metastases from the intratubular germ cell neoplasia unclassified type that may mature at the metastatic sites to a specific germ cell tumor type (2).
Patients with advanced choricocarcinoma have a worse prognosis than do the patients with other advanced/poor prognosis non-seminomatous GCTs because of the very high levels of hCG and the propensity for pulmonary and non-pulmonary visceral metastases (8). Batata (9) reported on a series of pure choriocarcinomas with no long-term survivors. Jensen and Venner (10) presented data from a population of 77 advanced germ cell patients who were treated with cisplatin-based therapy, and 3 of 77 patients had pure choriocarcinoma. All the three patients with pure choriocarcinoma died. The recurrent pure choriocarcinoma also has a very poor prognosis. There has been a report on a large series from Indiana University of 135 patients with GCTs and these patients failed after the first-line, platinum-based therapy, and the patients were treated with standard salvage chemotherapy with vinblastine, ifosfamide and cisplatin. Thirty-two patients were long-term survivors, but all the seven choriocarcinoma syndrome patients died (11). However, Papiani and Einhorn (8) reported that long-term survival and a potential cure was possible with high-dose chemotherapy in the patients with recurrent choriocarcinoma. The patients with choriocarcinoma who fail to achieve a complete response (CR) to the first-line therapy (the so-called incomplete responders) have a less than a 10% likelihood of long-term survival with the second-line chemotherapy (12-14). Our case had residual pulmonary nodules, which was pure choriocarcinoma, after combination chemotherapy. Therefore, we performed high-dose chemotherapy together with autologous stem cell transplantation without biopsy of the residual disease. In summary, we report here a rare case of a mixed testicular germ cell tumor that presented as metastatic pure choriocarcinoma, and this patient achieved continuous remission for 2 years after combination chemotherapy of BEP and sequential high-dose chemotherapy.