Life-Sustaining Treatment States in Korean Cancer Patients after Enforcement of Act on Decisions on Life-Sustaining Treatment for Patients at the End of Life
Article information
Abstract
Purpose
In Korea, the “Act on Hospice and Palliative Care and Decisions on Life-sustaining Treatment for Patients at the End of Life” was enacted on February 4, 2018. This study was conducted to analyze the current state of life-sustaining treatment decisions based on National Health Insurance Service (NHIS) data after the law came into force.
Materials and Methods
The data of 173,028 cancer deaths were extracted from NHIS qualification data between November 2015 and January 2019.
Results
The number of cancer deaths complied with the law process was 14,438 of 54,635 cases (26.4%). The rate of patient self-determination was 49.0%. The patients complying with the law process have used a hospice center more frequently (28% vs. 14%). However, the rate of intensive care unit (ICU) admission was similar between the patients who complied with and without the law process (ICU admission, 23% vs. 21%). There was no difference in the proportion of patients who had undergone mechanical ventilation and hemodialysis in the comparative analysis before and after the enforcement of the law and the analysis according to the compliance with the law. The patients who complied with the law process received cardiopulmonary resuscitation at a lower rate.
Conclusion
The law has positive effects on the rate of life-sustaining treatment decision by patient’s determination. However, there was no sufficient effect on the withholding or withdrawing of life-sustaining treatment, which could protect the patient from unnecessary or harmful interventions.
Introduction
With the development of modern medicine, it is possible to treat or control many diseases, thereby extending the human lifespan. However, life-sustaining treatment for patients who are unlikely to recover may interfere with the dignified dying of patients. Therefore, ethical and legal issues regarding the process of determining and implementing appropriate life-sustaining treatment have risen. Laws on withholding or withdrawing life-sustaining treatment have been enforced in several countries to ensure dignified death [1,2]. In Korea, since the case at Boramae Medical Center in 1997 and the case of “Grandma Kim” in 2008 [3], there has been increasing debate about patient self-determination regarding life-sustaining treatment at the end-of-life. After several social discussions and consensus processes, the “Act on Hospice and Palliative Care and Decisions on Life-sustaining Treatment for Patients at the End of Life” was established on February 2016 and enacted on February 4, 2018 [4]. After the enforcement of the law, patients at the terminal phase of disease or end-of-life can legally withhold or withdraw life-sustaining treatment, including cardiopulmonary resuscitation, hemodialysis, and the use of mechanical ventilation or chemotherapy. The purpose of the act is to protect the dignity and value of human beings by ensuring the best interests of the patients at the terminal phase of disease or end-of-life and by respecting their self-determination.
In the law, the requirements for withholding or withdrawing life-sustaining treatment involve several steps. The first step is the assessment of the patient at the end-of-life or with terminal illness. The doctor in charge and one medical specialist in a medical institution with an ethics committee must assess the person as a patient nearing death, who have no chance of recovery despite treatment, and rapidly worsening symptoms. The second step is a verification of the decisions of the patient or patient’s family. The patient or patient’s family member should express that the patient does not want life-sustaining treatment using advance directive on life-sustaining treatment, life-sustaining treatment plan, verification of consistent statements of two or more family members or unanimous consensus of the patient’s family members. And then, it should be verified by the doctor in charge and one medical specialist. Finally, life-sustaining treatment can be withheld or withdrawn only if there is a medical assessment that the patient is in the end stage of life, and the patient’s intention to avoid life-sustaining treatment is verified [5].
After the law was implemented, it is necessary to investigate whether the law have been applied properly and if the purpose of the law has been achieved. Although single-center experiences have been reported after the enforcement of the law [6,7], it is necessary to investigate the status of life-sustaining treatment in Korea. For this reason, we analyzed the data from the National Health Insurance Service.
Materials and Methods
1. Study patients
Cancer death data were derived from the National Health Insurance Service from November 2015 to January 2019. These were extracted from cancer patients and confirmed deaths during the period according to the Korean Standard Classification of Diseases and V codes. In Korea, cancer patients registered with the National Health Insurance Service receive V codes. The accuracy of the method of searching for cancer patients using both the Korean Standard Classification of Diseases and the V code is very high. Cancer deaths were divided into three groups: “before the law”, cancer deaths before enforcement of the life-sustaining treatment decisions act; “compliance with the law”, cancer deaths complied with the law process; and “non-compliance with the law”, cancer deaths did not follow the law process. Cancer death data during the national pilot project period (from November 2017 to January 2018) before enforcement of the life-sustaining treatment decisions act were excluded from the analysis.
2. Data collection and statistical analysis
Demographic data (sex, age, location) and social economic variables (income rank, death) were collected from a qualification database. Treatment database of medical institutions were used to classify the cancer type (type of disease, 40T); claim for life-sustaining treatment decisions; prescription of life-sustaining treatment including chemotherapy, mechanical ventilator, hemodialysis, cardiopulmonary resuscitation; and use of medical institutions (details of treatment, 30T) during the last 6 months before death. Charlson comorbidity index was estimated by summing weights of 17 defined comorbidities using Quan’s algorithm [8], when claimed for any visit of predefined International Classification of Diseases diagnosis during previous 1 year of death. The clinical characteristics were summarized as frequency (proportion), median, and range. Statistical analyses were performed with SAS version 9.4 (SAS Institute Inc., Cary, NC).
Results
1. Analysis of the demographic and socioeconomic characteristics in the last month before death
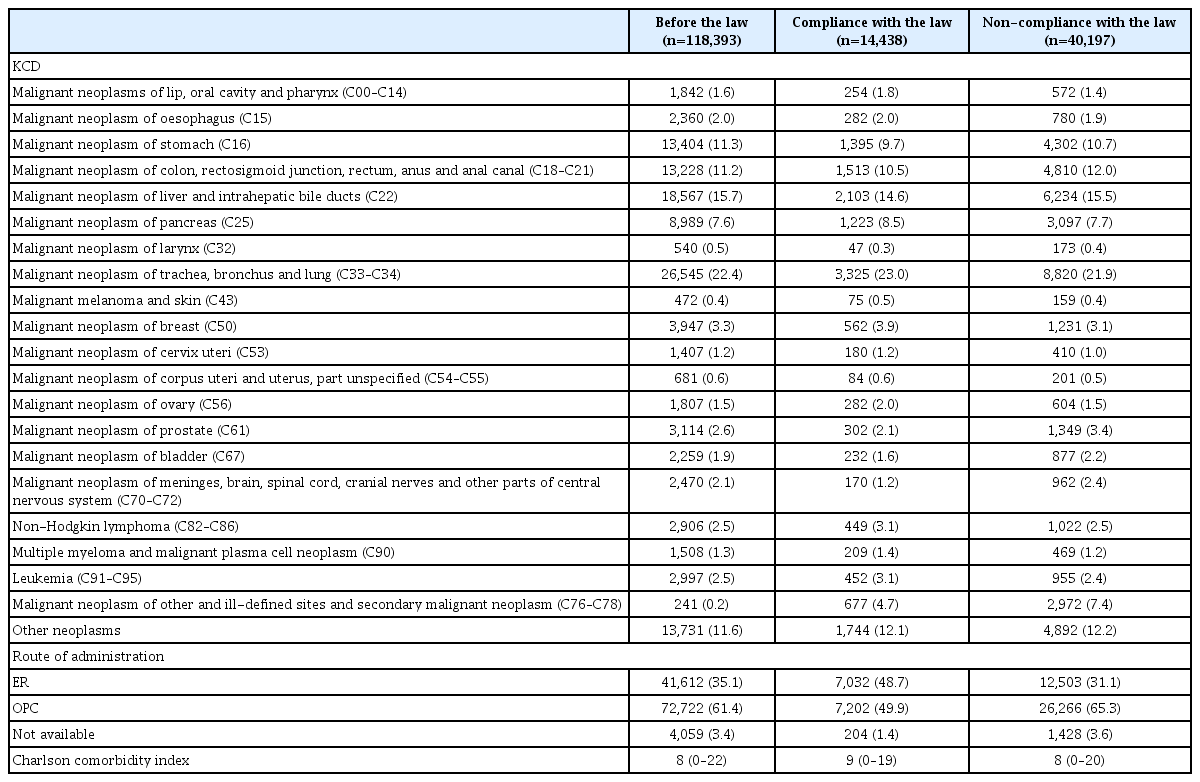
Between November 2015 and January 2019, the data of 173,028 cancer deaths were used in the analysis. Among them, 54,635 cancer deaths came after the enforcement of the law. The number of cancer deaths that complied with the law process was 14,438 out of 54,635 cases (26.4%). Of these, 7,078 patients (49.0%) had written an advance statement on life-sustaining treatment (life-sustaining treatment law appendix form No. 10: 397 patients) or life-sustaining treatment plan form (life-sustaining treatment law appendix form No. 1: 6,747 patients). Sixty-six patients had written both forms. The cancer deaths with an advance statement on life-sustaining treatment or life-sustaining treatment plan forms could be classified as a life-sustaining treatment decision by patient self-determination. Therefore, the rate of patient self-determination was 49.0%. Demographic and socioeconomic characteristics of the patients are shown in Table 1. After the enforcement of the law, the proportion of non-compliant cancer deaths was lower in patients under age 65 (age < 65, 66.1% [10,673/16,143] vs. age ≥ 65, 76.7% [29,524/38,492]; p < 0.001). However, there was no difference in the analysis according to sex. The regions where the law compliance rate exceeded the national average were in Ulsan (44.3%), Incheon (39.0%), Jeju Island (38.4%), Seoul (37.4%), Gwangju (30.0%), Jeollanam-do (29.3%), Sejong (27.5%), and Gyeonggi-do (26.8%). There was no significant difference according to income. Most of the cancer deaths occurred in general hospitals, including secondary and tertiary hospitals. After enforcement of the law, 12,665 out of 36,451 cancer patients (34.7%) treated in general hospitals complied with the law process. However, the compliance rate of primary hospitals and nursing hospitals were only 12.4% and 7.7%, respectively.
2. Analysis of medical data in the last month before death
The descriptive analysis of medical data in the last month before death is shown in Table 2. The proportion of cancer types that complied with the law was highest in the order of lung cancer, liver and biliary tract cancer, stomach cancer, and colorectal cancer. In the analysis of compliance with the law within a specific cancer group, 32.1% of skin cancer deaths and 32.1% of leukemia cancer deaths complied with the law process, followed by ovarian cancer (31.8%), breast cancer (31.3%), head and neck cancer (30.8%), and multiple myeloma (30.8%). However, the central nervous system cancer (15.0%) has the lowest compliance, followed by prostate cancer (18.3%), and bladder cancer (20.9%). It was found that the compliance with the law process of patients admitted through the emergency room was better than those admitted through an outpatient clinic (36.0%, 7,032/19,535 vs. 21.5%, 7,202/33,468, p < 0.001). Most of the patients (64.8%) have been treated by physicians in the department of internal medicine. Among 35,398 patients treated by internal medicine specialists, 10,849 cancer deaths (30.6%) complied with the law process. In contrast, 14.8% (678/4,579 patients) and 23.0% (1,836/7,989 patients) of cancer deaths in the surgery departments and family medicine complied with the law process.
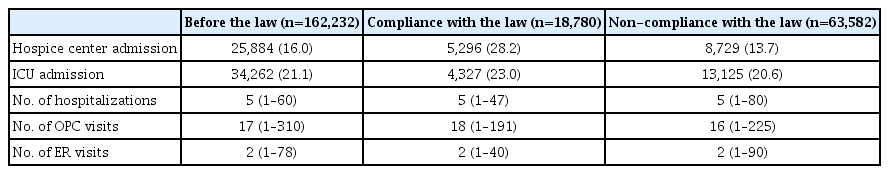
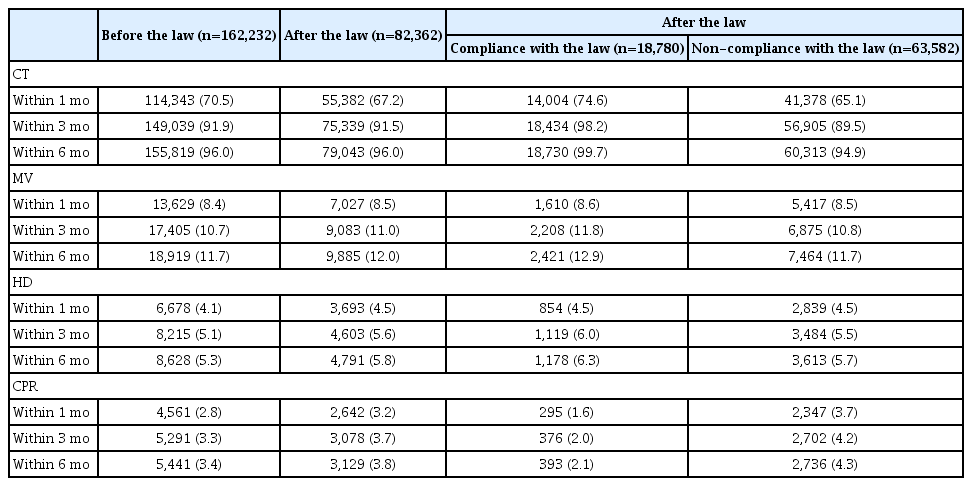
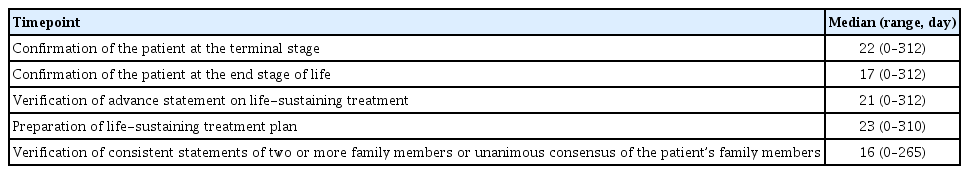
3. Analysis of the use of medical institutions and life-sustaining treatments within 6 months before death
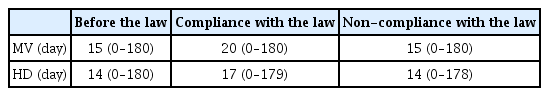
The patients complying with the law process had used a hospice center more frequently (“compliance with the law” 28% vs. “non-compliance with the law” 14%, p < 0.0001). However, the rate of intensive care unit (ICU) admission was similar between compliant and non-compliant patients (ICU admission, 23% vs. 21%, respectively) (Table 3). Before the enactment of the law, 70.5% of patients received chemotherapy within one month before the date of death. On the other hand, 67.2% of the patients received chemotherapy after the enforcement of the law. However, there was no significant difference in the analysis of results within 3 months (before the law 91.9% vs. after the law 91.5%) and 6 months before the date of death (before the law 96.0% vs. after the law 96.0%). When the law was enacted, it was found that patients who complied with the law process received more active chemotherapy during the last six months. There was no difference in the proportion of patients who had undergone mechanical ventilation and hemodialysis in the comparative analysis before and after the enforcement of the law and the analysis according to the compliance with the law. There was no significant difference in the proportion of patients who received cardiopulmonary resuscitation before and after the enforcement of the law, but after the enforcement of the law, patients who complied with the law process received less cardiopulmonary resuscitation (Table 4). In patients who complied with the law process, the interval between the date of last life-sustaining treatment and the date of death was longer than those who did not comply with the law process or those who died before the enforcement of the law (Table 5). The analysis of the time from life-sustaining treatment decisions to death is shown Table 6.
Discussion
According to the analysis data of the National Agency for Management of Life-Sustaining Treatment, as of November 2020, 130,237 decisions on life-sustaining treatment by patients or family members had been registered, and the implementation of withholding or withdrawing of life-sustaining treatment has also increased monthly [9]. In the present study, despite the enforcement of the law, only 26% of the cancer patients made the life-sustaining treatment decision in accordance with the law. It is possible that the rest of the patients died without a life-sustaining treatment decision or died after a decision by other means such as a do-not-resuscitate form. This finding is similar to a previous study before the enforcement of the law. In a study before the law was enacted, it reported the findings on whether life-sustaining treatment decision forms could be applied in the actual oncological practice. An et al. reported that among 336 cancer patients, Physician Orders for Life-sustaining Treatment (POLST) forms were introduced to 60.1% of patients, and 31.1% signed the form. Physician barriers were reluctance of the family, lack of rapport, patients’ denial of prognosis, lack of time, feelings of guilt, and uncertainty about either prognosis or the right time to discuss POLST. The patient’s barriers were lack of knowledge about POLST, emotional discomfort, difficulty in making decisions, or denial of prognosis [10]. In 2016, when the enforcement of the law was announced, a study to investigate awareness and attitudes toward advance care planning in Korea reported that a total of 15% of the general population, 33% of the patients and caregivers, and 61% of the physicians had knowledge of advance directives [11]. From these results, Koreans lacked awareness regarding the process of discussing medical care and determining life-sustaining treatment at the end-of-life. Unfortunately, even in these circumstances, there were not enough preparation, promotion, and education before the law was implemented. After the law was implemented in 2018, the physicians, patients, and family members were confused and spent lots of time and effort in the process of complying with the law process, such as filling out forms rather than ensuring patient self-determination and dignity in death. In addition, the law came into force in the absence of sufficient preparation for individual hospitals. In the present study, life-sustaining treatment decision in accordance to the law was higher in general hospitals (34.7%) than in primary hospitals (12.4%) and nursing hospitals (7.7%). Although most of the cancer deaths occurred in general hospitals, many patients with terminal phase cancer were also receiving end-of-life care at primary hospitals or nursing hospitals in Korea. However, because the law has strict conditions on hospitals that can make life-sustaining treatment decisions, most primary hospitals and nursing hospitals could not provide end-of-life care according to the law. In January 2019, general hospitals that can make life-sustaining treatment decisions according to the law was 38.8% (137/353 hospitals). However, only 0.6% (9/1,465 hospitals) of primary hospitals and 1.4% (22/1,560 hospitals) of nursing hospitals had a legal system for life-sustaining treatment decisions. Until recently, this situation did not improve significantly (In November 2020, general hospital, 55.0% [199/362 hospitals]; primary hospitals, 1.4% [22/1,518 hospitals]; nursing hospitals, 4.4% [69/1,585 hospitals]) [9]. The law designed for a dignified death needs to streamline its process to achieve their objectives and adjust the relevant regulations.
Nevertheless, there were positive effects of the law on the process of preparing for death in Korea. Our results showed that 49% of the patients decided on life-sustaining treatment by patient self-determination. In a single-center report collected after the enforcement of the life-sustaining treatment decision act, 44.2% of the cancer patients completed the documents for life-sustaining treatment decision and were written by the patient themselves [6]. However, another retrospective study reported a lower rate. Among 809 patients, 231 patients (29%) completed the forms themselves, and 578 (71%) had family members complete the forms [7]. According to the analysis data of the National Agency for Management of Life-Sustaining Treatment, the proportion of patients with or without cancer that made life-sustaining treatment decision by patient’s determination is steadily increasing (until January 2019, 32.3% [11,615/35,994 patients]; until November 2020, 35.8% [46,575/130,237 patients]) [9]. Before the life-sustaining treatment decision law was enforced, the life-sustaining treatment decision was usually made using the do-not-resuscitate form in accordance with the regulations of each hospital. Previous studies have reported that life-sustaining treatment decisions through the do-not-resuscitate form have been mainly made by the patient’s family members [12,13]. However, according to the life-sustaining treatment decision act, if a patient can express his or her own intentions, only the patient can decide on life-sustaining treatment. As a result, patients, family members, and physicians had to include patients in the life-sustaining treatment decision process, and it became important to confirm the patient’s intentions for life-sustaining treatment decisions. The law has led to a change in the culture of life-sustaining treatment decisions in Korea, and as a result, it can be expected that the rate of patient self-determination will gradually increase.
Prior to the enforcement of the law in Korea, discussions and decisions about life-sustaining treatment were made near the date of death [14]. In the present study, most of the patients had prepared the life-sustaining treatment decision form within one month before the date of death. Late life-sustaining treatment decisions lead to unnecessary and harmful treatments to the cancer patient, thereby adversely affecting the patient’s quality of life and dignified death [15,16]. Moreover, there is a tendency to perform aggressive anti-cancer or life-sustaining treatment as the end-of-life approaches [17]. In previous studies, 30.9% of cancer patients received chemotherapy [18] and 33.6% visited an emergency room more than once during the last months [19]. In contrast, only 9.1% of patients were referred to a hospice consultation service at the end-of-life period [19]. In the present study, life-sustaining treatment decision complying with the law was associated with increased use of hospice center. However, there was no significant difference in ICU admission between compliant and non-compliant patients. Contrary to expectations, the ICU admission rate was not affected by the life-sustaining treatment decision act. This result is consistent with previous studies [7,17]. In a previous study, the ICU admission rate within the last month before death in patients with terminal cancer was 30.3%. Of note was that the ICU admission rate was lower when life-sustaining treatment was decided by the patient than when decided by family members [7]. In the present study, the patient self-determination rate was 49%. Therefore, if the rate of life-sustaining treatment decisions made by the patient rises in the future, it can be expected that the implementation of life-sustaining treatment such as ICU admission will be decreased. From a different point of view, Korean patients, family members, and physicians have tended to decide whether to perform cardiopulmonary resuscitation mainly among various life-sustaining treatments. In the present study, the proportion of patients receiving mechanical ventilation or hemodialysis within six months before death was similar between patients who decided on life-sustaining treatment and those who did not. However, the proportion of patients who received cardiopulmonary resuscitation was lower in those who complied with the law. This trend has been reported in previous studies. Although the rate of admission to the ICU within the last month before death is high, the rate of cardiopulmonary resuscitation is relatively low [7,12]. In addition, according to the 2019 annual report on the life-sustaining treatment decision system by Korea National Institute for Bioethics Policy, the rate of withholding or withdrawing of life-sustaining treatment was 99.4% for cardiopulmonary resuscitation, 86.5% for mechanical ventilation, 83.4% for hemodialysis, and 60.6% for chemotherapy [20]. Therefore, physicians need to explain and discuss various life-sustaining treatments in the process of making life-sustaining treatments decision with patients at the terminal disease or end-of-life.
This study could be used as basic data on the application of the law and its effects in the early period of law enforcement. In addition, this study provides large-scale analysis data on the past and current status of life-sustaining treatment for cancer patients. Based on these basic data, it is possible to find optimal directions for the improvement of the shortcomings of the law and related policies. Nevertheless, this study has some limitations. First, because it is based on the large data from the National Health Insurance Service, it is impossible to investigate the detailed life-sustaining treatment decision process of individual patients. Second, there may be a difference of several days between the time point used for the analysis of the study and the time point applied at the time of actual decision or treatment. Third, it was impossible to distinguish patients who had life-sustaining treatment decision but had a missing insurance claim. Fourth, since the same claim code was assigned to the withholding and withdrawal, it was not possible to distinguish between withholding and withdrawal of life-sustaining treatment.
In summary, despite the law being enforced, only some cancer patients complied with the law process. Nevertheless, the law has positive effects on the rate of life-sustaining treatment decision by patient’s determination. However, there was no sufficient effect on the withholding or withdrawing of life-sustaining treatment, which could protect the patient from unnecessary or harmful interventions. As the shortcomings of the law are corrected and understanding of patients and physicians is improving, it is expected that the purpose of the life-sustaining treatment decision law will be gradually reached. Therefore, this study needs to be repeated at regular intervals.
Notes
Ethical Statement
This study was reviewed and approved by the Ethics Committee of the National Evidence-Based Healthcare Collaborating Agency (NA19-008) and the Kangdong Sacred Heart Hospital (2019-12-013), which waived the need for informed consent because of the descriptive nature of this study and no personal information included.
Author Contributions
Conceived and designed the analysis: Won YW, Kim HJ, Kwon JH, Lee HY, Baek SK, Kim YJ, Kim DY, Ryu H.
Collected the data: Kim HJ, Kwon JH.
Contributed data or analysis tools: Won YW, Kim HJ, Kwon JH, Lee HY, Baek SK, Kim YJ, Kim DY, Ryu H.
Performed the analysis: Won YW, Kim HJ, Kwon JH.
Wrote the paper: Won YW, Kim HJ, Kwon JH.
Conflicts of Interest
Conflict of interest relevant to this article was not reported.
Acknowledgements
This study was supported by a grant from the National Evidence-based Healthcare Collaborating Agency (NA19-008).