Effect of Dose Escalation with Single Opioid, Fentanyl Matrix in Patients Not Controlling Cancer Pain: A Multicenter, Prospective, Observational Study in Korea
Article information
Abstract
Purpose
End-of-dose failure (EOD) is a clinically common observation and many cancer patients increase the frequency of opioid administration. Fentanyl matrix use is known to be effective in patients with chronic cancer pain. To measure the effectiveness of increase in a single dose of fentanyl matrix in patients whose pain was not controlled sufficiently, we perform this study.
Materials and Methods
A multi-center, open-label, prospective, observational study was conducted in 30 hospitals in Korea, between August and December 2008.
Results
A total of 452 patients were enrolled; 404 patients completed the study. The mean pain intensity decreased from 5.27 at the first visit to 3.37 at the end of the trial. There was a significant difference in pain intensity (p < 0.001) between the first and last visits. The percentage of pain intensity difference was 30.1%. The prevalence of EOD at the first visit was 73% from the 452 enrolled patients. After the use of fentanyl patch, EOD decreased from 73% to 56%. Pain intensity of patients experiencing EOD was 5.64 at the baseline compared to 4.27 in patients without EOD. On final visit, pain intensity in patients with and without EOD was 4.02 and 2.54, respectively. The observed adverse events were mainly nausea, asthenia, constipation and diarrhea.
Conclusion
This study demonstrated that increasing dose of fentanyl patch decreased pain intensity and decreased the rate of patients experiencing EOD. Thus, fentanyl patch may be an effective modality in cancer patients whose pain was previously not controlled sufficiently; the side effects were as could be expected with an opioid.
Introduction
Treatment of cancer pain is one of the most important goals of palliative medicine [1,2]. However, alleviation of pain is often a difficult problem to solve. Opioid drugs are the principal agents used to control pain in cancer patients [3-5]. If pain in patients with progressing cancer is worsened or constant, medical staff needs to recognize the necessity of increasing the analgesic dose of opioids. However, despite the World Health Organization (WHO)'s recommendation, the reality is that pain is not satisfactorily controlled in 30% to 50% of patients complaining of cancer pain [6,7].
The most likely reason for not using sufficient analgesics is the fear of analgesic-induced adverse events or shortening of patients' life expectancy [8]. The answer can be found in a study of end-stage patients receiving hospice treatment at home [1]. With regard to life expectancy of cancer patients, as well as their demographics, clinical data, and especially their pathology, the study researched correlation with necessity of high-dose morphine administration. According to the results, use of a high-dose of morphine did not have an effect on shortening the life expectancy of patients and could be safely used as pain treatment.
In general, strong opioid analgesics do not have a ceiling effect. Thus, clinicians can increase the dose without limit, if and when they determine that it is beneficial to control the pain. Combined use of opioid analgesics is not generally recommended in real practice, and this method of opioid analgesic use may be due to the fear of high-dose opioid analgesic use or is considered a sign of wrong clinical judgment [9].
Although the baseline chronic pain is well controlled, some cancer patients suffer from transient exacerbation of pain, known as episodic or breakthrough pain. In general, breakthrough pain is managed by a search of the factors and removing them as much as possible, and short acting opioid drugs may be added to a regular opioid treatment [10,11]. On the other hand, if sustained analgesic drugs can not sustain efficacy, it can result in induction of breakthrough pain. This is known as end-of-dose failure (EOD), which is one type of breakthrough pain [12,13]. From clinical experience, EOD of long acting morphine, oxymorphone, and oxycodone has been commonly observed [12]. Results of a survey of patients with chronic pain provided clarification that EOD of long-acting oxycodone is the primary reason that patients take more analgesic than recommended by the manufacturer. In a study of patients with chronic pain, who were taking long-acting oxycodone, methadone, or morphine, Gallagher et al. [14] found that many patients were taking more analgesics than the recommended dose in their package inserts, and in addition, were taking a rescue opioid analgesic 3 to 4 times more that the recommendation, but still could not sufficiently control pain.
Fentanyl matrix is a transdermal drug delivery system that provides continual delivery of fentanyl for 72 hours. The use of fentanyl matrix, if needed in higher dosages, is known to be effective in controlling pain in patients with chronic cancer pain [15,16]. Therefore, in this study, we evaluated the effectiveness of a single dose escalation of the fentanyl matrix on pain control in patients whose pain was not sufficiently controlled with the use of previous analgesic in real practice via the investigator's discretion. The results of this study will strengthen the basis for clinical usefulness of the fentanyl matrix for controlling cancer pain.
Materials and Methods
This multicenter, open-label, prospective, observational study was conducted at 30 sites in Korea, from August 2008 to December at 2008. The study protocol was approved by the Institutional Review Board of each site, and the study was conducted in accordance with the Korean requirement for execution of clinical trials, International Conference on Harmonisation Good Clinical Practices guidelines, and Decalaration of Helsinki.
The study population included patients who visited study center during the study period with a complaint of cancer pain and were receiving a monotherapy or combination therapy of sustained-release oral strong opioid analgesics, but failed to control pain sufficiently and needed an increase in their dose of the fentanyl matrix via the investigator's discretion. In order to participate in this study, subjects were required to satisfy the following criteria: 1) patients aged 20 years or older; 2) patients complaining of pain with a score of 4 or more on the numeric rating scale (NRS), requiring administration of opioid analgesic; 3) patients who were not satisfied with pain control despite a monotherapy of a sustained-release oral strong opioid analgesic or combination therapy of a sustained-release oral strong opioid analgesic and fentanyl matrix; and 4) patients who signed the informed consent form. On the first visit day (visit 1), we changed the previous opioid drug to fentanyl patch of equivalent dose. Dose equivalence was calculated using the 1:3:2 durogesic patch to morphin to oxycodon ratio. Demographic data, patients' primary tumor, metastasis, and stage, as well as other disease characteristics, such as previous analgesics including name, dosage, pain intensity, frequency of EOD, and degree of sleep disturbance were documented. Sleep disturbance was described according to the NRS from 0 (not disturbing at all) to 10 (very disturbing). Over a period of approximately one month, we adjusted the patients' daily dose of fentanyl matrix depending according their pain control by National Comprehensive Cancer Network (NCCN) guidelines. On visit 2 (day 29±7), any adverse events that the subject had experienced since visit 1 were recorded. In addition, pain intensity applied the fentanyl patch dosage, frequency of EOD, and degree of sleep disturbance and evaluated the effectiveness of the study drug in patients during the study period according to the investigator's judgment (Investigator's Global Assessment) and patient's judgment (Patient's Global Assessment), and how the patients' condition was improving, compared to visit 1 (Clinical Global Impression-Improvement [CGI-I]) (Fig. 1).

Study design. On the first visit, we changed the previous opioid drug to fentanyl patch of equivalent doses. Further, we surveyed the demographic data and patients' primary tumor, metastasis, stage, and etc. Over a period of approximately one month, we adjusted the patients' daily dose of fentanyl matrix, depending on their pain relief. On the second visit (day 29±7), we performed a reevaluation of the items described above.
The primary objective of the study was to demonstrate the clinical usefulness of the fentanyl matrix by measuring its pain control effects after an increase of a single dose of fentanyl matrix in patients whose pain was not sufficiently controlled with the use of previous analgesic in real practice via the investigator's discretion.
The secondary objective was to observe improvement in the following variables after treatment with fentanyl matrix: sleep disturbance caused by pain, Investigator's and Patient's Global Assessment, patient's satisfaction, and CGI-I. In addition, adverse events occurring during the study period were investigated.
T-test, Wilcoxon rank-sum test, and chi-square test were used for testing the statistical differences in demographic data and health condition. Differences between before and after administration of the study drug were tested using a paired t-test, Wilcoxon signed rank test, Wilcoxon rank-sum test, chi-square test, and etc. according to the characters of endpoints.
Results
1. Patient characteristics
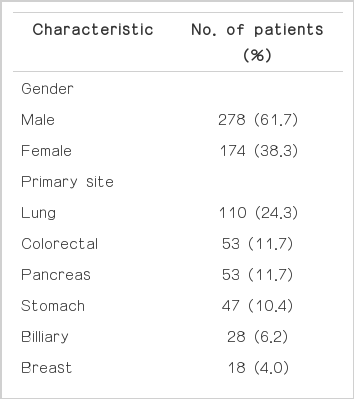
A total of 452 patients were enrolled in the study. However, 48 patients dropped out. Therefore, a total of 404 patients completed the study. Characteristics of patients are shown in Table 1. Of the 452 enrolled patients, 61.7% were male. The average age was 63.2 years. The principal primary diagnosis was lung cancer (24.3%), colorectal (11.7%), and pancreas (11.7%). The majority of these patients were stage IV (85%); 46% of patients kept pace with cancer treatment: chemotherapy (84%) and radiotherapy (11%).
2. Efficacy parameter analysis
The mean pain intensity at the first visit was 5.27 (±1.953), and 3.37 (±1.986) at the second visit day. A significant difference was observed in pain intensity between the first and second visits (p<0.001) (Fig. 2). The percentage of pain intensity difference was 30.1%. In addition, we evaluated sleep disturbance of pain according to the scale (not disturbing at all in 0, very disturbing in 10). Sleep disturbance scale for the first visit was 3.69 and for the second visit was 2.55. The percentage of patients who woke up one or more times decreased from the first to the second visit (71.5% vs. 59.9%).
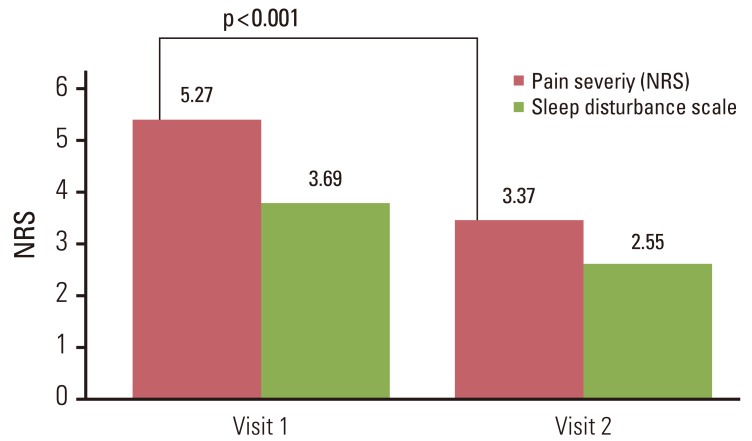
Pain intensity and sleep disturbance scale on visit 1 and visit 2. The mean pain intensity of the first visit was 5.27 and that of the second visit was 3.37. A significant difference was observed in two pain intensities (p<0.001). Further, the mean sleep disturbance scale of the first visit and the second visit was 3.69 and 2.55, respectively. However, this was not statistically significant. NRS, numeric rating scale.
The prevalence of patients who experienced an EOD at the first visit was 73% of the 452 enrolled patients. The oxycodon medication group accounted for the largest portion of patients who experienced the EOD (65%). The oxycodone with the fentanyl patch group and the morphin controlled release (CR)-treated group accounted for 26.9% and 6.5% of patients, respectively, who experienced an EOD. We investigated the existence of EOD according to the type previously used analgesics. The oxycodon or oxycodone combination group showed a larger portion of EOD than the morphin or morphin combination group (approximately 70% vs. 50%). At the second visit, the proportion of EOD decreased, from 73% to 56% (Fig. 3).
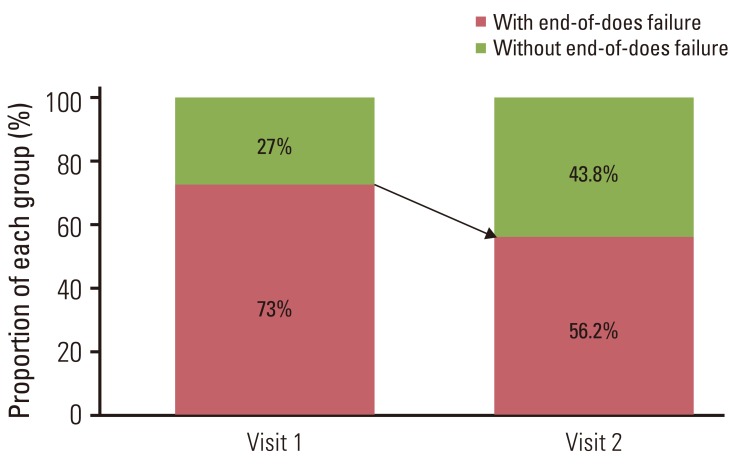
The proportion of end-of-dose failure on visit 1 and visit 2. After the use of fentanyl patch, the proportion of end-of-dose failure showed a reduction, from 73% to 56.2%.
Pain intensity in patients with EOD was 5.64, in patients without EOD was 4.27 at the first visit; the difference was statistically significant (p<0.01). On the second visit, pain intensity in patients with EOD and without EOD was 4.02 and 2.54 (Fig. 4), which was statistically significant (p<0.01). The sleep disturbance scale was 4.15 in patients with EOD at the first visit, and 2.43 in patients without EOD (Fig. 4); these results showed statistical significance (p<0.01). Patients with EOD had less satisfaction with pain control than patients without EOD (satisfaction rate 9.4% vs. 32.8%), and it was statistically significant (p<0.01). The mean initial dose of fentanyl matrix was 45 mcg/day (range, 12 to 350 mcg/day) on the first visit. On the second visit, of the 404 completed patients, a mean dose of fentanyl matrix was 55.6 mcg/day (range, 12 to 625 mcg/day). The number of patients who increased the dose of fentanyl patch was 93; otherwise, the number of patients decreased dose of fentanyl patch was 6. A statistician rate of Investigator's Global Assessment was 66.0%, and that of the Patients' Global Assessment was 63% (Fig. 5). The rate of pain improvement was 33.7% by CGI-I. Of the 404 patients, 64 patients (14.2%) reported adverse events (AEs), the most frequent AEs of associated drugs included nausea, asthenia, constipation, and diarrhea (Table 2). Serious adverse events (SAEs) were observed in 19 patients (4.19%). The majority of SAE was death, not related to the fentanyl patch. Other SAEs included another cancer occurrence and neutropenia, also not related to the fentanyl patch.

The pain intensity and sleep disturbance scale with or without end-of-dose failure (EOD). Pain intensity of patients who had experienced EOD and those who had not experienced EOD was 5.64 and 4.27, respectively, on the first visit. On the second visit, the pain intensity of patients who had experienced EOD and those who had not experienced EOD was 4.02 and 2.54, respectively. The sleep disturbance scale of patients who had experienced EOD and those who had not experienced EOD was 4.15 and 2.43, respectively on the first visit. On second visit, the sleep disturbance scale of patients who had experienced EOD and those who had not experienced EOD was 3.15 and 1.77, respectively. Pain intensity and sleep disturbance in patients with EOD between that of patients without EOD was statistically significant on the first and second visits. NRS, numeric rating scale.

Satisfaction rate of Investigator's Global Assessment and Patient's Global Assessment. The satisfaction rate of the Investigator's Global Assessment was 66.0%, and that of the Patient's Global Assessment was 63%.
Discussion
Since the WHO cancer treatment guidelines were announced (1986), pain management for cancer patients has shown steady progress. Many opioid drugs have been developed, and adequate relief of cancer-related pain has been reported in 70-97% of cancer patients [17-20].
Some studies have reported that although analgesics were administered at the physician's discretion, many patients felt pain prior to the next dose of medication (that is EOD). Adams et al. [21] investigated the frequency of sustainedrelease opioid dosing in patients with chronic benign pain: Dosing more frequently than every 12 hours was documented in 70.6% and 86.8% of morphin CR-treated and oxycodon treated patients, respectively. However, only 23.9% of patients in the transdermal fentanyl patch-wearing group were self-medicated every 48 hours, rather than every 72 hours [21]. According to the results of another study conducted for investigation of dosing frequency of sustained-release opioids in patients with chronic, nonmalignant pain, 91% of oxycodone CR-treated patients, 86% of morphin CR-treated patients, and 50% of fentanyl patch-treated patients were self-medicated more frequently than the manufacturer's recommendation [14]. Regarding chronic malignant cancer pain, another group recently conducted a survey of dosing frequency of oral sustained-release opioids or transdermal fentanyl; 26.2% of oral sustained-release oral opioid patients took their medication more than twice per day, and 11.2% of fentanyl patch wearing patients wore the patch every 48 hours, rather than 72 hours [22]. The results of these surveys suggest that despite controlling pain using opioid drugs, many patients felt pain, and especially complained of EOD, also, suggesting that EOD caused an increase in dosing frequency, and patients treated with the fentanyl patch had lower incidence of EOD than those treated with an oral opioid drug. Therefore, we thought that the fentanyl patch may be helpful in the management of uncontrolled cancer-related pain. Thus, we evaluated the effectiveness of fentanyl matrix in patients whose pain was not sufficiently controlled by investigating the pain intensity, frequency of EOD, degree of sleep disturbance, and degree of satisfaction with pain control after the use of fentanyl patch.
Our data indicate that the fentanyl patch was effective for the management of patients with uncontrolled cancer-related pain via a statistically significant reduction of pain intensity. Also, in our study, the rate of patients who experienced EOD was 73% with administration of oral opioid or oral combination of opioid and fentanyl. Patients who experienced end-of dose failure were intended to have score higher on the pain intensity scale (5.64 vs. 4.27) and sleep disturbance scale (4.15 vs. 2.43) than patients without EOD. Therefore, the results of our study suggests that EOD may have an association with the quality of life, and thus, decreasing EOD is helpful to supportive care of cancer patients.
After the use of fentanyl patch, the EOD rate appeared to diminish (73% to 56.2%), and pain intensity showed a significant decrease, from 5.27 to 3.37. These facts suggest that the fentanyl patch may be effective, and can be considered as another option for treatment of poorly controlled cancerrelated pain. Further, sleep disturbance scale showed a decrease, from 3.69 to 2.55. However, this result was not statistically significant. The satisfaction rate of Investigator's Global Assessment was 66.0%, and that of the patients' global assessment was 63%. The rate of pain improvement was 33.7% by CGI-I. According to the results described above, the use of fentanyl patch may result in a decrease in EOD and pain intensity, as well as an increase in the rate of satisfaction with pain control. This fact, that satisfaction rate increases after the use of fentanyl patch, suggests that the fentanyl patch may be helpful in enhancing the quality of life.
The observed adverse events associated with the use of fentanyl patch were mainly nausea, asthenia, constipation, and diarrhea. However, the side effects were not much different from the use of an opioid with use of an opioid, and were manageable.
We concluded that the fentanyl patch is a useful treatment option in patients with insufficient pain control. However, our study was limited due to its open-label, observational design. Therefore, a future double-blinded randomized trial to evaluate the effectiveness of the fentanyl patch is warranted.
Conclusion
The results of this study suggest that the fentanyl patch may be an effective drug for controlling cancer-related pain in patients whose pain was previously not controlled sufficiently with morphine only or morphine combination. In addition, the fentanyl patch may be helpful in reducing EOD with an improvement of quality of life. The side effects were not much different from the use of an opioid.
Acknowledgments
This research was supported financially by grants from the Johnson and Johnson family of companies whose role was restricted to providing assistance to the investigators in the conception, conduct, and analysis of this study.
Notes
Conflict of interest relevant to this article was not reported.