Current Practice and Barriers in Cancer Rehabilitation: Perspectives of Korean Physiatrists
Article information
Abstract
Purpose
The purpose of this study was to assess clinical practice and barriers associated with cancer rehabilitation from the perspective of Korean physiatrists.
Materials and Methods
All active members of the Korean Academy of Rehabilitation Medicine were invited to complete an online survey developed after focus group discussions.
Results
A total of 97 physiatrists (72 males and 25 females) in Korea completed the survey. Of these, 77% reported familiarity with the term 'cancer survivors.' More than 50% of respondents reported that they provided rehabilitation services for patients with breast cancer (61.9%), brain tumors (64.9%), and spinal tumors (63.9%), whereas 86.6% of respondents reported that they had never or rarely provided rehabilitation programs for patients with gynecological, colorectal, or prostate cancer. Physiatrists who received referrals from a well-organized cooperative referral system reported providing services such as exercise programs for patients with gynecological cancer (odds ratio [OR], 2.16; p=0.044) as well as education regarding lymphedema (OR, 1.81; p=0.047) and neuropathic pain (OR, 1.96; p=0.026).
Conclusion
Although most of the physiatrists surveyed believed that they should contribute to the management of cancer patients, they considered themselves ill equipped to provide appropriate rehabilitation services. This lack of understanding of the effectiveness of rehabilitation services for cancer patients and absence of a cooperative referral system are the major barriers to providing rehabilitation services to cancer survivors in Korea.
Introduction
Early diagnosis and improved cancer treatments have increased the number of cancer survivors. Accordingly, cancer rehabilitation has been increasingly recognized as a key factor in the management of cancer survivors. Cancer rehabilitation involves helping cancer patients achieve maximum possible physical, social, psychological, and vocational functionality within the limits imposed by the disease and its treatment. Furthermore, rehabilitation plays a role in increasing interaction with the community [1]. Such care is based on the assumption that rehabilitation is a complex and long-lasting process involving interactions between patients, their relatives, and health professionals [2].
An integrated and cross-disciplinary approach is ideally suited for providing cancer patients meaningful benefits [3]. Multi-disciplinary rehabilitation services are naturally influenced by referral patterns, the range of available therapeutic options and services, as well as health care setting [4]. Physiatrists can influence treatment decisions [5] by informing and advising cancer patients, oncologists, and other primary caregivers. Thus, improved understanding of the barriers and opportunities related to cancer rehabilitation from the perspective of physiatrists is needed [6].
The organization and systems involved in rehabilitative care services differ markedly among countries [7]. Differences relating to funding, accessibility, and the definition of cancer rehabilitation services were recently noted in a review on current perspectives and emerging issues related to cancer rehabilitation in Europe and the United States [7]. Physiatrists have shown increasing interest in cancer rehabilitation and are playing an increasingly significant role in the care of cancer patients in Korea. However, to our knowledge, no studies have focused on rehabilitation services for cancer survivors from the perspective of physiatrists. Here, we conducted a survey to assess clinical practice and barriers associated with provision of cancer rehabilitation services from the perspective of Korean physiatrists. Our results may increase awareness of the role of physiatrists in supportive cancer care and highlight the need for collaboration among physiatrists in various countries.
Based on previous studies, expectations of oncologists regarding cancer survivorship care differ considerably from those of supportive care providers, underscoring the potential complexity of delivering consistent survivorship care [8]. Few studies have formally examined possible solutions to these discrepancies or evaluated intervention strategies for optimizing care [9]. The rehabilitation process is dependent on appropriate communication among health care sectors and should address unfulfilled needs of patients [10]. Thus, we investigated the perception of physiatrists regarding the effects of cooperation on the quality of cancer survivorship care as well as understanding of the rehabilitation requirements of cancer survivors.
This study assessed the perspective of Korean physiatrists with respect to rehabilitation of cancer survivors in terms of core content, clinical practice, attitudes, and barriers as well as examined factors that contribute to the optimal delivery of rehabilitation services.
Materials and Methods
1. Study design
The survey was conducted between May 2011 and August 2011. The questionnaire was the result of a collaborative effort among Korean physiatrists. Contact addresses of all physiatrists were obtained with the assistance of the Korean Academy of Rehabilitation Medicine (KARM). All members of KARM were invited to complete an online survey by selecting a web link provided in an email. Those interested in participating were directed to a website where they completed the online survey. The survey was administered from secure servers and was accessible by all potential respondents. A follow-up reminder email was sent to all potential participants 2 weeks later. The mean time required to complete the web-based survey was 30 minutes. The study protocol was approved by the Institutional Review Board of Seoul National University Bundang Hospital (Protocol No. B-1009/054-003).
2. Survey questionnaire
The questionnaire was developed by a focus group of Korean physiatrists specializing in cancer rehabilitation. The group discussed the priorities of rehabilitation services for cancer survivorship in terms of content, clinical practices, attitudes, and barriers, including environmental factors such as governmental support, financial support, and medical equipment, during three consecutive online and offline meetings. The questionnaires were developed based on these discussions, pilot-tested, and revised.
The survey covered the following domains: personal and professional characteristics, recognition of range of rehabilitation services, common rehabilitation services for general and cancer-type-specific dysfunctions, attitudes toward cancer rehabilitation, and perceived barriers to cancer rehabilitation.
The range of rehabilitation services was evaluated by the question “During which phase(s) of the cancer continuum are rehabilitation services provided?” Response choices included ‘initial phase of diagnosis,’ ‘treatment phase,’ ‘post-treatment phase,’ ‘follow-up phase without recurrence,’ ‘advanced cancer phase,’ and ‘end-of-life stage.’
Knowledge of common rehabilitation services for general and cancer-type-specific dysfunctions was evaluated by 24 questions, with responses based on a five-point Likert scale (‘none,’ ‘a little,’ ‘some,’ ‘a lot,’ and ‘all’). Respondents were asked to rate the quality and importance of each of the rehabilitation services provided to their patients.
The respondents were then asked to describe their perception of the hospital environment as well as organizational culture regarding cancer rehabilitation services. In this domain, the respondents were surveyed on whether or not their hospital had a built-in referral system, frequency of referrals for specific reasons, and timing of referrals in the cancer trajectory. Our survey examined the barriers to delivery of rehabilitation services to cancer patients, including lack of knowledge of services or referral mechanisms, lack of information about cancer rehabilitation among cancer patients, lack of perception of importance of cancer rehabilitation by oncologists and physiatrists, lack of governmental support such as subsidized medical costs, lack of financial support, and lack of medical equipment. Respondents rated each item using a five-point Likert scale, with a score of ‘1’ indicating that the factor was ‘always’ a barrier and ‘5’ indicating that the factor was ‘never’ a barrier.
The survey provided information on the demographic and practice characteristics of respondents. In our analysis, we considered the following variables: age, sex, proportion of cancer patients among all patients treated by physiatrists, and type of medical institution according to function and number of beds; local clinics (primary), hospitals (secondary), general hospitals (secondary), or total care general hospitals (secondary and tertiary).
3. Statistical analyses
Characteristics, attitudes, perceived barriers to care, and perceived preparedness of respondents were analyzed as categorical outcomes and frequencies. For the analyses, the ‘all,’ ‘a lot,’ and ‘some’ responses were grouped together as ‘usually or always,’ whereas ‘a little’ and ‘none’ responses were grouped as ‘never or rarely.’ The referral system from oncologists was dichotomized (having vs. not having). For the preparedness variables, response categories were dichotomized into ‘unprepared (1-2)/prepared (3-5).’ The barriers to care variables were dichotomized into ‘moderate/big problem’ versus ‘no/small problem.’ A multivariable logistic regression model was constructed to examine factors associated with delivery of rehabilitation services. After adjusting for age, sex, institution, and proportion of cancer patients, we entered several potential factors into the model, including knowledge of the benefits of rehabilitation services for cancer patients, referrals for cancer rehabilitation services by oncologists, and available physiatrist services. The odds ratios (ORs) and 95% confidence intervals were determined. All tests were two-sided, and p-values of < 0.05 were deemed to be statistically significant. All statistical tests were conducted using the SPSS ver. 17 (SPSS Inc., Chicago, IL).
Results
1. Participants
All members of the Korean Academy of Rehabilitation Medicine (n=1,194 physiatrists) were identified and invited to participate in the study. Of these, 1,189 physiatrists were contacted, and a total of 171 responses were received for an overall response rate of 14.4%. Reasons for the low response rate are not clear, but it may be that members were deceased, retired, or practicing in other countries, using default email addresses, spam filters, or lacked interest in the survey. The 171 physiatrists who agreed to participate logged into the Internet Platform, and 97 responses were used in the analysis since the remaining 74 did not respond to all questions. Of these 97 physiatrists, 74% of respondents were male and ~95% were aged 30-49 years. Further, 5.1% of respondents practiced in primary care sectors, 35.1% practiced in secondary care sectors, and 59.8% practiced in tertiary general hospitals (Table 1).
2. Definition of cancer survivors and range of rehabilitation services
The proportions of physiatrists experienced in treating cancer patients were 5.2% in the initial diagnosis phase, 25.8% in treatment phase, 39.2% in post-treatment phase, 22.7% in follow-up phase (without recurrence), 42.3% in advanced cancer stage, and 26.8% in ‘end-of-life’ stage. In response to questions about the cancer care continuum, 77% reported having heard the term ‘cancer survivors.’ More than 80% of physiatrists perceived ‘cancer survivors’ as individuals in the ‘after treatment’ and ‘follow-up without recurrence’ phases, whereas those ‘with advanced cancer’ were considered to be cancer survivors in need of cancer rehabilitation services. Further, 84.5% of physiatrists reported that patients were recipients of at least some type of rehabilitation service during ‘treatment phase.’ Furthermore, 78% of physiatrists agreed that cancer patients in the ‘end-of-life’ stage needed rehabilitation services.
3. Rehabilitation services for cancer-related dysfunctions
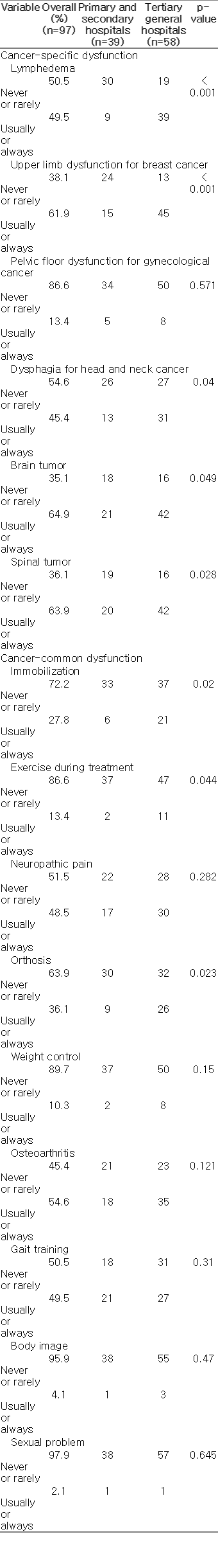
In response to questions on the availability and delivery of rehabilitation services for cancer-specific dysfunctions, more than 50% of respondents reported that they provided rehabilitation services for patients with breast cancer (61.9%), brain tumors (64.9%), and spinal tumors (63.9%), whereas 86.6% reported never or rarely providing rehabilitation services for patients with gynecological, colorectal, or prostate cancer. Services that physiatrists considered very important but did not provide to their patients were mobilization (importance, 90.0%; delivery, 27.8%), exercise during cancer treatment (importance, 82.1%; delivery, 13.4%), weight control programs (importance, 69.2%; delivery 10.3%), and sexual rehabilitation (importance, 63.2%; delivery, 2.1%) (Table 2).
Only 32 respondents (33%) reported receiving referrals from oncologists to their departments of rehabilitation medicine. Reasons for referrals, in decreasing order, were lymphedema (85.6%), pain (84.6%), disabilities in performing daily living activities (66.0%), gait disturbance or dysphagia (64.9%), exercise (53.6%), and orthosis or prosthesis (48.5%). Of those who had a referral system at their hospitals, referrals received from oncologists were for patients in the initial phase of diagnosis (12.5%), treatment phase (34.4%), posttreatment phase (53.1%), follow-up phase without recurrence (31.3%), advanced cancer stage (68.8%), and ‘end-of-life’ stage (31.3%).
4. Barriers to cancer rehabilitation
Commonly cited barriers to delivery of rehabilitation services were lack of knowledge about benefits of rehabilitation services for cancer patients (87.6%), lack of awareness of cancer rehabilitation services among oncologists (85.6%), and lack of a uniform service module among physiatrists (51.5%). Over 80% of respondents reported a lack of governmental support, such as health delivery systems or health policies (96.9%), financial support (92.8%), and medical equipment (86.5%), as barriers to cancer rehabilitation.
We also measured a significant difference between respondents who were trained as cancer rehabilitation physiatrists in the delivery of upper limb rehabilitation programs for women with breast cancer versus those who were not (OR, 2.41; p=0.041). Respondents who reported that their work setting had a referral system from oncologists reported providing care such as exercise programs for gynecological cancer (OR, 2.16; p=0.044) as well as information on lymphedema (OR, 1.81; p=0.047) and neuropathic pain (OR, 1.96; p=0.026) more often than those working in hospitals without an effective referral system (Table 3).

Multivariate analysis of perception of cancer rehabilitation and likelihood of providing rehabilitation services (odds ratios)
Additionally, female physiatrists provided more rehabilitation services for lymphedema (OR, 2.81; p=0.035) than their male counterparts. However, we found no significant sexbased differences in the delivery of other cancer rehabilitation services in Korea.
Discussion
We surveyed Korean physiatrists to assess their understanding of the benefits of cancer rehabilitation as well as the availability and delivery of rehabilitation services to cancer survivors in Korea. We defined “cancer survivor” as any individual with cancer. Until know, information on issues surrounding the delivery of cancer rehabilitation in Korea has been scarce. The majority of physiatrists recognized that cancer patients in the trajectory from initial diagnosis to ‘ end-of-life’ required rehabilitation services, and they identified multiple areas of care delivery needing improvement. Although most agreed with basic precepts such as the importance of rehabilitation services, the majority reported deficiencies in the delivery of these services. Barriers identified by physiatrists were related to lack of knowledge about cancer rehabilitation by patients, oncologists, and physiatrists. More than 80% of physiatrists in our study cited governmental support, financial support, healthcare equipment, and medical facilities as necessary to support rehabilitation services in Korea.
We also found differences in the availability and delivery of rehabilitation services according to type of cancer. Rehabilitation services for patients with breast cancer and central nervous system tumors were provided by more than 50% of physiatrists. However, other services such as pelvic floor rehabilitation programs for patients with gynecological cancer, colorectal cancer, and prostate cancer, exercise and mobilization programs during cancer treatment, weight control programs, and sexual rehabilitation were provided by less than one third of physiatrists, although most considered these services necessary for cancer patients. Previous studies from Western countries have reported that cancer patients often experience a number of problems that require rehabilitation services, including general weakness and pain [11,12], and patients’ functional status can be improved following rehabilitation [13].
Our definition of ‘cancer survivor’ involved an individual’s journey from the moment of diagnosis to the end of his/her life, as cancer survivors experience different problems according to the stage of their disease [14]. A recent study estimated that up to 10% of cancer survivors are in the rehabilitation phase at any given time [15]. In our study, most physiatrists considered patients who had completed treatment with no obvious recurrence as ‘cancer survivors,’ although they perceived patients in the ‘during treatment’ or ‘end-of-life’ stage as needing cancer rehabilitation services. Social stigma is attached to the Korean word for ‘survivor,’ which means a person who has managed to stay alive after suffering a difficult situation as a result of being unlucky or as a form of punishment. Cancer patients in Korea are reluctant to be called ‘survivors’ since it suggests that they are unlucky or are being punished. Thus, a ‘person who experienced cancer’ is a more acceptable phrase in Korea than ‘cancer survivor.’
There are various definitions of cancer rehabilitation, alternate indicators of cancer rehabilitation, and varying levels of access to those services both within and among countries, reflecting different funding systems and widening health inequalities. In Korea, interest in cancer survivorship has increased since the late 2000s, and the field of cancer rehabilitation is undergoing rapid development. The perceived discrepancy between the range of treatment phases that require cancer rehabilitation and the availability and delivery of those services may be explained by the lack of promotion of cancer survivorship and education in Korea. The term ‘cancer survivor’ is not publicly used in medical practice. However, changing social attitudes in Korea may diminish this discrepancy.
Our study showed that rehabilitation services were provided more frequently for breast, brain, and spinal cancers than for other types of cancer. In contrast, recognition levels of pelvic floor rehabilitation programs, exercise education, and sexual rehabilitation were low. There were also discrepancies between the perceived importance and delivery of rehabilitation services, particularly for general cancer-related dysfunctions such as fatigue [16]. Jo et al. [16] conducted a survey on Korean cancer patients and found that patients experienced various cancer- and treatmentspecific physical, psychological, and socioeconomic problems, thus displaying a strong need for rehabilitation services. Our data highlight the importance of developing effective and efficient rehabilitation programs that are specific to each phase of cancer survivorship.
In this study, respondents provided moderate to high quality rehabilitation services for breast cancer patients with upper-limb dysfunction (lymphedema). This finding indicates that specific dysfunction and rehabilitation services must be understood for successful cancer rehabilitation. As supportive care for cancer survivors becomes more advanced and its scope of practice expands, physiatrists should have a good understanding of cancer-related disabilities and treatment protocols. In addition to factors related to physiatrists, communication between oncologists and physiatrists, including transfer of patients from primary cancer treatment to supportive care, remains problematic. The clinical load is actually increasing on a relatively small group of oncology professionals who have little to no information regarding rehabilitation services for physical impairments, such as contracture, weakness, and deconditioning [17]. Physiatrists understand the pathophysiologies of fibrosis, deficits in muscle strength and flexibility, lymphatic insufficiency, muscle hypertonicity, and neural hypersensitivity, all of which require supportive care [18]. However, these dysfunctions appear to be under considered in the Korean health system. Early diagnosis and empirically based prevention of functional problems will limit long-term functional and psychological morbidity [19]. Thus, measurement of functional problems by physiatric evaluation during the early and most treatable stages of cancer is critical.
Levels of rehabilitation services provided to patients are influenced by the referral system and the hospital. Our findings revealed a statistically significant increase in services provided by physiatrists who worked in hospitals where oncologists referred patients for rehabilitation. The relationship between oncological and rehabilitation specialties may be important to initiate and coordinate the cancer rehabilitation process [19]. Furthermore, a referral system is necessary to refer patients for relevant rehabilitation activities [20]. The quality of rehabilitation services is likely dependent on referral patterns, team communication, and effective rehabilitation treatment processes [21]. The reluctance of oncologists in referring patients to physiatrists could be related to a lack of evidence of the benefits of cancer rehabilitation programs or inefficient patient referral processes. A systemic review examining barriers preventing access to supportive and palliative care has identified a lack of knowledge among health professionals, a lack of standardized referral criteria, and difficulty in equitable access to services [22]. Thus, the development of guidelines that specifically address supportive care should be considered [23]. Most previous studies on rehabilitation services have focused on patients, and a few have surveyed primary physicians; however, to our knowledge, none has surveyed physiatrists. A previous study revealed that 35% of European medical oncologists have collaborated with supportive care specialists, and of those, 88% felt that oncologists should coordinate supportive care for their patients [2]. Another survey of Australian cancer specialists showed that that 48% of respondents referred more than 60% of their patients to supportive care services [10]. In the present study, only one-third of physiatrists received referrals from oncologists, two-thirds of which were for patients in the “after treatment” phase or those with advanced cancer. The referral system should allow referrals of patients before and during treatment for early detection of problems as well as to provide effective rehabilitation services. The results of our survey suggest that oncologists in each field must be informed about rehabilitation services. Moreover, a lack of preparation for rehabilitation services was perceived as a barrier in Korea. Lack of governmental support, such as absence of a delivery system, limited standard guidelines for service delivery and monitoring, poor financial support for insurance coverage, and lack of medical equipment may severely restrict the delivery of rehabilitation services for cancer survivors.
The professional qualifications of personnel involved in cancer rehabilitation and palliation vary worldwide [24]. Compared with physiatrists in other countries, Korean physiatrists have played a leading role in founding and managing the Korean Research Council of Cancer Rehabilitation. Although our study revealed Korean physiatrists have a relatively low level of cancer rehabilitation knowledge and operate within an inactive referral system, they are aware of the need for cancer rehabilitation services and have specific and relevant knowledge of both general and cancer-type-specific dysfunctions.
1. Limitations
Several factors should be considered in the generalization of these findings. Our study was designed to assess the perspective of physiatrists in Korea with the goal of encouraging physiatrists to discuss their role in supportive cancer care according to the circumstances of each country. A high percentage of physiatrists contacted via email did not respond. Since the reasons for this are unknown, we cannot excluded any resulting biases. Moreover, self-selection bias limits the generalization of these results to all physiatrists. However, the sex and age distributions of the respondents were similar to the average of Korean physiatrists. We recruited participants from a sample of physiatrists in Korea; thus, a survey of the perspectives of participants from different professional and cultural backgrounds is needed. To evaluate the effectiveness of oncologist referral systems, it is crucial to understand the perspective of oncologists as well as compare it with that of physiatrists. In conjunction with the survey on physiatrist recognition and attitudes, we interviewed oncologists of various specialties as primary cancer care professionals by means of semi-structured questionnaires, and a comparison study of the perspectives of oncologists and physiatrists is ongoing (unpublished data).
Conclusion
Although most of the physiatrists surveyed believed that they should contribute to the management of cancer patients, they considered themselves ill equipped to provide appropriate rehabilitation services. Poor understanding of the effectiveness of rehabilitation services in cancer patients and lack of a cooperative referral system are the major barriers to providing rehabilitation services to cancer survivors in Korea.
Notes
Conflict of interest relevant to this article was not reported.
Acknowledgements
This study was supported by a grant from the National R&D Program for Cancer Control, Ministry of Health & Welfare, Republic of Korea (08-2010-047) and a grant from the Seoul National University Bundang Hospital Research Fund (02-2011-028). The authors are indebted to J. Patrick Barron, Professor Emeritus, Tokyo Medical University and Adjunct Professor, Seoul National University Bundang Hospital for his pro bono editing of this manuscript.