A Case of Medullary Thyroid Carcinoma in which the Skin Metastasis was Concurrently Present and Response Occurred to Chemotherapy
Article information
Abstract
Medullary thyroid carcinoma accounts for 3% of all thyroid gland malignancies. It commonly metastasizes to liver, lung, and bone. It rarely metastasizes to skin, and only a few such cases have been documented. Cutaneous metastasis suggests a poor prognosis, with a mean survival of 7.5-19 months. The most effective treatment for skin metastasis is complete surgical removal of all local and regional lesions. The response to systemic chemotherapy is typically poor. We report a case of medullary thyroid carcinoma with cutaneous metastases, which responded to chemotherapy.
INTRODUCTION
Cases in which the specific primary cancer metastasizes to the skin have rarely been reported and this is indicative of disseminated cancer. Skin metastasis of thyroid cancer has been relatively rarely reported. Most of the cases include papillary cancer and follicular one (1). In cases of medullary cancer, accounting for 3~10% of total thyroid carcinomas, skin metastasis has been reported in several cases up to the present (2~4,6). Due to a lack of treatment response, no satisfactory treatment outcomes have been reported even following surgical resection, radiotherapy and anti-cancer chemotherapy (2~4).
We experienced a patient with medullary thyroid carcinoma in whom myriads of red or purple, flat-buldged nodular metastatic lesions accompanied by the notable hyperkeratinized papule and macule in the adjacent area to the neck or anterior chest area. In this patient, we performed anti-cancer chemotherapy without surgical resection. Nevertheless, this patient showed a treatment response for a certain period of time. Here, we report our case with a review of literatures.
CASE REPORT
A 74-year-old man presented with a gradual increase of the size and number of palpated nodules in the neck eight years prior to his outpatient visit. At other institution, the patient underwent needle aspiration cytology, histopathologic analysis and computed tomography in 2003. This led to the diagnosis of lymphoma or metastatic carcinoma with unknown primary site. Thereafter, he received one-time anti-cancer chemotherapy (carboplatin 450 mg/gemcitabine 2,000 mg). Following this, while the patient was maintaining the lives without further receiving the examination and treatment, the mass accompanied by the tenderness around the bilateral neck and anterior chest area appeared approximately six months. The patient therefore visited us in about April of 2006. On physical examination, the patient had a flash on the face. In the bilateral adjacent area to the neck and the anterior chest area, myriads of red or purple, flat-buldged nodular metastatic lesions accompanied by the notable hyperkeratinized papule and macule were present. To identify the primary site, F-18 FDG positron emission tomography-CT was performed. This detected multiple hypermetabolic masses in the bilateral thyroid glands, the soft tissue in the neck and lung as well as the enlargement of cervical, axillary and medistinal lymph nodes with hypermetabolism. On CT scans of the chest and neck, multiple lymph node enlargement, granuloma or metastatic lesions were identified (Fig. 2). A histopathologic analysis of the cervical lymph node showed that a poorly-differentiated metastatic carcinoma was present. On a fine needle aspiration cytology of thyroid gland, the presence of thyroid medullary carcinoma was suspected. A subsequent histopathologic examination of skin lesions on the left neck also detected a poorly-differentiated metastatic carcinoma, based on which the multiple metastases, including the skin, of thyroid medullary cancer were strongly suspected. Besides, on immunohistochemistry of both cervical lymph node and skin lesions, there were calcitonin-positive staining properties (Fig. 4). Serum calcitonin level was 208 pg/ml (normal range: 0~10 pg/ml) and serum CEA level was 144.4 ng/ml (0~5 ng/ml), both of which were elevated. Thyroglobulin was 31.8 (0~52 ng/ml) and this was within the normal range. To make a differential diagnosis of the concurrent presence of multiple endocrine adenomas, the test was performed. This showed intact PTH 17.10 pg/ml (15~65 pg/ml), Metanephrine 0.2 mg/day (-0.8 mg/day) and VMA 2.9 mg/day (0~8 mg/day) on a 24-hr urinalysis, which were all normal.

A computed tomography of the neck (contrast enhancement) (A, B) Several lymph nodes which were non-specifically enlarged were observed in bilateral neck areas. (B) A low-density area which was suspected to be cancer was observed in the right lobe of thyroid gland.

Histopathologic and immunohistochemical findings. (A) A fine needle aspiration biopsy: Aggregates of tumor cells having enlarged & hyperchromatic nuclei which are suggestive of the possibility of medullary carcinoma of the thyroid gland. (B) Cervical lymph nodes: Mostly replaced by tumor cells. Tumor cells infiltrated into the adjacent soft tissue. (C) The soft tissue around the lymph nodes: Tumor featuring a calcitonin-positive staining property. (D) Metastatic skin lesions of the neck: Tumor featuring a calcitonin-positive staining property
From June 20 of 2006 to May 31 of 2007, the patient received a total of 13 times of anti-cancer chemotherapy, starting with the intravenous infusion from days 1 to 5 using dacarbazine (250 mg/m2) and 5-FU (450 mg/m2) at a cycle of 28 days. As compared with the time point of initial hospitalization, the flash almost disappeared. A follow-up PET-CT showed that the size of metastatic lesions such as the neck, axillary lymph node and other soft tissue areas was decreased (Fig. 1, 3). Of the nodules with a various size, the largest one had a size of 2.5×1.5 cm2. From the fifth anti-cancer treatment on, the size was decreased. Following the twelfth treatment, most of the nodules disappeared. The nodule with a greatest size was decreased to 0.8×0.6 cm2. The patient was recommended to receive the surgical treatment for the remaining (residual?) mass during the anti-cancer chemotherapy, but refused. Serum calcitonin and CEA levels were persistently decreased until the sixth anti-cancer treatment, which were noted to be 76.9 pg/ml and 43.1 U/ml, respectively. Following this, these levels were increased at a minimal amount. After the treatment was discontinued, they were abruptly increased (Fig. 5). Following the 13th anti-cancer chemotherapy, the patient refused to take the treatment. From the second month following the discontinuation of treatment, the size of skin lesions and various lymph nodes was gradually increased. Six months following the discontinuation of treatment, the patient preseneted with delirium symptoms. On brain MRI scans, multiple brain metastasis was noted. In January of 2008, the patient was expired. Before then, the patient had survived up to 27 months following the onset of skin metastasis.

The decreased size of metastatic skin lesions (A) prior to chemotherapy (B) on the 4th cycle following the chemotherapy (C), (D) on the 13th cycle following the chemotherapy (the largest nodule, from 2.5×1.5 cm2 to 0.8×0.6 cm2)
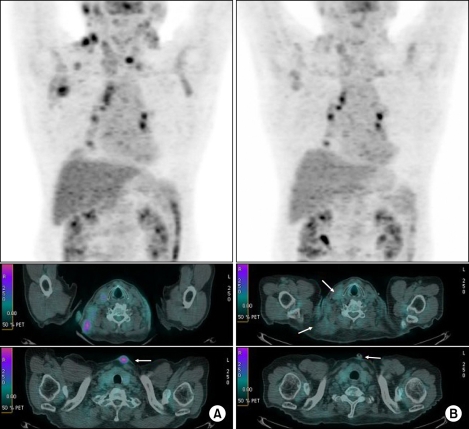
FDG PET/CT scan. (A) Initial scan showed multiple hypermetabolic foci in the neck, mediastinum and axillary lymph nodes including borderline hypermetabolism of the right lobe of thyroid gland. (B) A follow-up scan (following the 5th chemotherapy) showed decreased metabolism & size in neck masses including axillary lymph nodes.
DISCUSSION
Thyroid medullary carcinoma is a tumor that originates from thyroid parafollicular cells which produce and then secrte calcitonin, and it accounts for approximately 1~3% of total cases of thyroid carcinomas in Korea. Organs where the distant metastasis is well developed include lung, liver and bone. It has been known that the metastasis to cervical lymph node is seen in approximately 50% of total patients and the distant metastasis is seen in approximately 5~10% of patients at the time of diagnosis. Unlike the tumors originating from follicular cells, including papillary cancer and follicular cancer, the treatment cannot be made with the use of radioactive iodine. It has been reported that the surgical resection of tumor including the lymph node is the only treatment regimen which can be recommended as a radical therapy. In addition, other treatment regimens such as the postsurgical radiotherapy, a single or compound chemotherapy of doxorubicin, somatostatin-analogue, the inhibitor of tyrosine kinase and radioactive immunotherapy. However, there were no significant evidences demonstrating the treatment effect. A 10-year survival of thyroid medullary cancer is approximately 60~70%. Particularly in cases of MEN2B and sporadic cases of thyroid medullary cancer, the prognosis has been reported to be poorer. A 5-year mortality rate has also been reported to be 30~50% (5).
The skin metastasis in cases of thyroid medullary cancer has been rarely reported to such an extent as to be described in approximately ten cases up to the present. Also in the current case, as seen in English literatures, the patient visited us with chief complaints of neck mass and skin lesions. In this patient, because the primary site was suspected to be thyroid carcinoma, a fine needle aspiration biopsy was performed. This revealed findings suggestive of thyroid medullary cancer. Serum calcitonin was elevated. In the metastatic skin lesions and the neck lymph nodes, an immunohistochemistry showed a calcitonin-positive result. These findings were indicative of the skin metastasis of thyroid medullary carcinoma. According to the reports that have been made until now, the skin metastasis was restricted to nodules and a mass. It has also been described that the skin lesions had a granulation tissue like nodules. As particularly seen in the current case, however, no cases in which hyperkeratinized nodules or a mass were present have been reported.
PET-CT scans, which were performed to identify the primary site, detected hypermetabolic foci in the skin lesions and the enlarged thyroid gland. These findings were helpful for making a diagnosis of multiple metastases of poorly differentiated thyroid carcinoma and were also useful in following up of treatment response to anti-cancer chemotherapy.
The skin metastasis of thyroid carcinoma is a disseminated tumor, and it has a poor prognosis to such an extent that its mean survival is at most 7.5~19 months (3,4). To date, due to a small number of cases of thyroid medullary cancer, a statistical significance could not be analysed. It is assumed, however, that the prognosis of thyroid medullary cancer would be poorer than predicted based on the characteristics of a tumor. According to two cases in which the chemotherapy was performed, Ordonez et al. performed the surgical resection as well as the chemotherapy comprising doxorubicin, cisplatinum and dacarbazine. But these authors did not concretely describe the treatment response. Alwaheeb et al. performed the chemotherapy and the external radiation therapy. These authors reported, however, that the initial level of serum calcitonin was 251 pg/ml and this showed no changes thereafter. They also noted that the metastatic skin nodules had an approximately 50% decrease (2,3). To date, in most of the cases, prior to the diagnosis of thyroid carcinoma and skin metastasis, the surgical resection of thyroid gland and radical neck dissection have been performed. Of four cases in which the death was reported, except for one case, the survival period did not elapse a year following the diagnosis of skin metastasis. In the current case, however, a mass was palpated in the neck eight years prior to outpatient visit. Six months prior to outpatient visit, the metastatic lesions were indentified in the skin around the neck. With a single use of the chemotherapy, the size of metastatic skin nodules and lymph nodes was decreased. Levels of CEA and calcitonin were also decreased during an approximately 6-month period. Following the discontinuation of chemotherapy, the patient showed an abrupt elevation of serum levels of calcitonin and CEA and died of brain metastasis. However, the patient survived approximately 8~20 months longer than the mean survival of patients with thyroid carcinoma in whom the skin metastasis was concurrently present. Accordingly, as seen in the current case, the anti-cancer chemotherapy would be considered an active treatment that can improve the symptoms and prolong the life span in patients with thyroid carcinoma in whom the skin metastasis was concurrently present.
