Pseudoaneurysm Due to Squamous Cell Carcinoma of the Lung: Two Cases of Spontaneous Resolution after Chemotherapy
Article information
Abstract
Pseudoaneurysm due to cancer is uncommon generally and is extremely rare in lung cancer. We report two cases of false aneurysms due to lung cancer that spontaneously regressed upon chemotherapy without intervention. Both patients had squamous cell carcinoma of the lung and the diagnosis of a pseudoaneurysm was made using computed tomography. There was no evidence of severe bronchial hemorrhage and the psuedoaneurysms were small and well-encased. Chemotherapy was performed and the pseudoaneurysms resolved.
Introduction
Pseudoaneurysm formation in pulmonary vasculature is a rare condition that is more common in females and in the elderly (1). Several etiologies have been described including tuberculosis, trauma, necrotizing pneumonia, congenital heart disease, and vasculitis (2). Pulmonary vasculature pseudoaneurysm formation is rarely related to cancer. We report two cases of pseudoaneurysm due to primary lung cancer as demonstrated by computed tomography (CT) that regressed after chemotherapy.
Case Report
Case 1
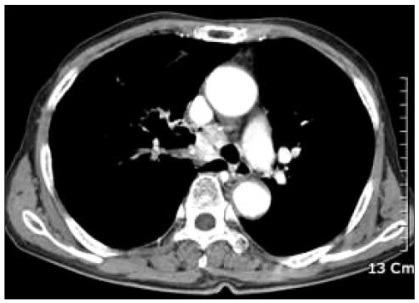
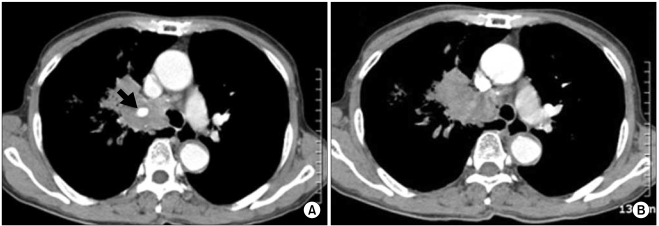
A 71-year-old Korean male presented with blood-tinged sputum, cough, and dyspnea that had lasted for 1 month. He had been treated for diabetes mellitus, hypertension, and congestive heart failure until 2 years prior to presentation. The patient was a tobacco smoker (50 packs of cigarettes annually) and no history of previous respiratory disease, trauma, or pulmonary intervention. The general physical examination was unremarkable except for diminished breath sounds in the left hemithorax. Blood pressure was 120/70 mmHg, pulse rate was 80 beats/min, and respiratory rate was 20 breaths/min. Hemoglobin level was 11.3 g/dL and oxygen saturation was 92%. The ejection fraction was 57%. A chest radiograph showed atelectasis in the left lower lobe. A contrast-enhanced CT scan revealed a 5.5×4.2 cm mass at the level of the carina with enhancement of the central part of the mass, which was not visible on the pre-enhancement CT (Fig. 1A). Enhancement was isodense with the pulmonary vasculature (Fig. 1B). Bronchoscopy demonstrated a protruding mass at the carina with near complete obstruction of the left main bronchus. A bronchoscopic biopsy from the mass revealed squamous cell carcinoma. The patient was transferred to another hospital for endobronchial stent placement, after which three cycles of combination chemotherapy using docetaxel and cisplatin were conducted. A follow-up CT scan showed a partial response of the primary cancer and resolution of the pseudoaneurysm within lung cancer (Fig. 2). No recurrent episodes of hemoptysis were noted.
CT observations for case 1. (A) Chest CT scan on admission demonstrated a central lung mass at the level of the carina, with no central enhancement within the mass in the pre-enhance CT. (B) A highly enhancing component within the mass was evident in the enhanced CT, similar in attenuation to that of the major vessels (black arrow).
Case 2
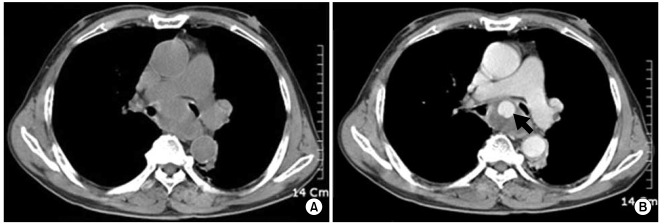
A 66-year-old Korean male presented with dyspnea and several episodes of minor hemoptysis lasting for 3 months. The patient was a tobacco smoker (70 packs of cigarettes annually) and had no significant medical history of trauma or pulmonary intervention. The physical examination was apparently normal. Blood pressure was 150/90 mmHg, pulse rate was 90 beats/min, and respiratory rate was 20 breaths/min. Hemoglobin level was 9.9 g/dL. A chest radiograph showed a diffuse and ill-defined patch of density in the right upper lobe. Contrast-enhanced CT in the arterial phase revealed a heterogeneously enhanced mass in the right upper lobe with a 1.4 cm sized lesion with strong enhancement in the center of the mass (Fig. 3A). The enhanced area was washed out in the delayed venous phase, consistent with an arterial pseudoaneurysm (Fig. 3B). Bronchoscopy demonstrated a large protruding mass obstructing the right main bronchus. Bronchoscopic biopsy of the mass revealed squamous cell carcinoma. A diagnosis of pseudoaneurysm with no risk of bleeding was followed by combination chemotherapy using docetaxel and cisplatin, as this regimen had a relatively low risk of thrombocytopenia. An enhanced CT scan obtained after the third cycle of chemotherapy showed a significant response and resolution of the pseudoaneurysm within lung cancer (Fig. 4).
CT observations for case 2. (A) Contrast-enhanced CT in the arterial phase revealed a heterogenous mass in the right upper lobe with a strongly enhancing 1.4 cm central area (black arrow). (B) The central enhancement was washed out in the delayed phase, compatible with a pseudoaneurysm of the artery.
Discussion
Pulmonary vasculature aneurysms and pseudoaneurysms are uncommon. Focal dilatation of the pulmonary artery can be congenital or acquired. Common causes include tuberculosis, pyogenic infection, trauma, and vasculitis (2). Pulmonary vasculature aneurysms and pseudoaneurysms associated with lung carcinoma are rare. We have found only three reports of pulmonary artery false aneurysms arising within a lung cancer (2-4); all were squamous cell carcinomas and the patients presented with massive hemoptysis. Consistent with a previous report (3), we speculated that pseudo-aneurysm in squamous cell carcinoma is associated with direct invasion and erosion of the vascular wall. The present cases displayed squamous cell carcinoma with hemoptysis associated with endobronchial mucosal ulceration.
In the past, the standard imaging technique for diagnosis of pseudoaneurym was pulmonary angiography, but this has now largely been superseded by CT angiography (1). CT can allow a precise definition of the extent of a pseudoaneurysm and associated mass. Pulmonary artery pseudoaneurysm appears as an enhanced round lung mass that is isodense to the central pulmonary arteries. Because pre-enhancement CT shows no central enhancement and the enhanced CT shows a highly enhancing component within the mass, a pseudoaneurysm within the pulmonary arterial system can be diagnosed. Since our cases had no massive hemoptysis, pulmonary angiography was not performed.
The treatment options for pseudoaneurysm include bronchoscopic coagulation, artery ligation, transcatheter embolization, lobectomy, and direct thrombin injection (4-6). Percutaneous transcatheter embolization is an alternative and less invasive form of treatment than open thoracotomy with resection (7). If a pseudoaneurysm is accompanied by massive hemoptysis, early recognition and treatment is important for reducing and preventing mortality, because mortality is 100% if the aneurysm ruptures (8).
Spontaneous resolution of pseudoaneurysm is possible for small forms and in a low-pressure environment (9). The pulmonary artery might differ from that of pseudoaneurysm in a high-pressure vessel such as renal, femoral, or popliteal arteries (9).
In our cases, the pseudoaneurysm was small and well-circumscribed without peripheral hemorrhage, and tightly encased within the cancer. Therefore, we reasoned that the pseudoaneurysm had less chance for rupture or massive hemorrhage. As the pseudoaneurysms resolved after chemotherapy, we pursued no further interventional procedures other than chemotherapy.
We have presented two cases of pseudoaneurysm associated with lung carcinoma. Our report is unique in that it is the first report in which pseudoaneurysm arising within lung cancer regressed in size following chemotherapy. Pulmonary circulation pseudoaneurysm should be considered in lung cancer cases with hemoptysis. But, if the patient has no massive hemoptysis and the pseudoaneurym is small in size, the patient should be carefully observed without interventional procedures. Further research is required to define the natural history and proper management for this medical condition.
Notes
This paper was supported by Wonkwang University in 2008.