Introduction
Leiomyosarcoma is a malignant soft tissue tumor that can arise from any tissue containing smooth muscle. However, leiomyosarcoma arising in paratesticular tissue is extremely rare and approximately only 10% of all paratesticular sarcomas are leiomyosarcomas [1]. The primary treatment for this tumor is radical orchiectomy with high cord ligation; however, the optimal local and systemic treatment remains controversial. Adjuvant radiotherapy is generally recommended for lowering the rate of local recurrence and the role of chemotherapy has not been fully established [2]. We report here on a case of stage III paratesticular leiomyosarcoma, which was treated successfully with orchiectomy and systemic chemotherapy.
Case Report
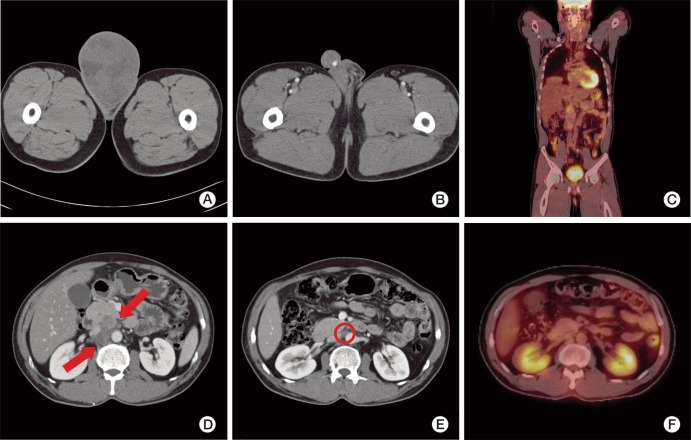
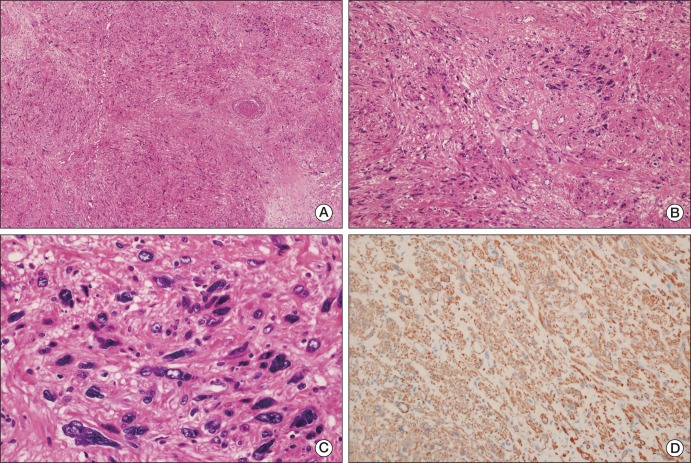
A 50-year-old male patient with a 10-year history of a huge right scrotal mass, which had shown rapid growth for more than one year, was referred to our department. Results of the physical examination revealed a right paratesticular mass measuring approximately 12 cm in diameter; the mass was firm and non-tender. The serum lactate dehydrogenase level was 313 IU/L, the α-fetoprotein level was 5.9 ng/mL, and the β-human chorionic gonadotropin level was 1.7 mIU/mL, which were all within the normal ranges. Findings on abdominal computed tomography (CT) showed a huge heterogeneous enhancing right scrotal mass (12×9 cm) with para-aortic and peri-caval lymphadenopathies (Fig. 1A and D). Right orchiectomy was performed and the macroscopic pathologic features showed a grossly intact testis with a well-defined, huge, whitish solid mass adjacent to the testis (Fig. 2). Immunohistochemical staining showed a positive result for smooth muscle actin (SMA), CD34, and desmin; however, immunostaining for myoglobin, S-100 protein, and c-kit showed a negative result. According to the pathologic results, the mass was characterized as a leiomyosarcoma, grade 3 (according to the French National Federation of Cancer Centers [FNCLCC] and National Cancer Institute [NCI] system): the total score was 8, the mitotic score was 3 (more than 20/10 high power field), the necrosis score was 2 (more than 50%), and the differentiation score was 3 (Fig. 3). According to the American Joint Committee on Cancer Sarcoma Staging system, this patient was stage III (T2aN1M0), therefore, we diagnosed the patient as having a stage III, grade 3 paratesticular leiomyosarcoma. The patient underwent additional systemic chemotherapy using ifosfamide 1 g/m2 on days 1 to 3 plus adriamycin 30 mg/m2 on day 1. Chemotherapy cycles were repeated every 21 days. After four cycles of chemotherapy, we performed abdominal CT for evaluation of the therapeutic response. The lymphadenopathies that were initially observed in the abdominal cavity had decreased in size by over 50% with no tumor recurrence, therefore, a partial response could be identified (Fig. 1B and E). After nine cycles of chemotherapy, whole body positron emission tomography-CT was performed and no uptake of fructose-1,6-bisphosphate (FDP) was observed (Fig. 1C and F). The patient has been followed up for 12 months after systemic chemotherapy, and he has consistently maintained a complete response (CR).
Discussion
Leiomyosarcoma is a soft tissue tumor arising from smooth muscle cells of a mesenchymal origin. Paratesticular leiomyosarcoma originates from the spermatic cord, the scrotum, or the epididymis. The most common type is the spermatic cord type, which arises from undifferentiated mesenchymal cells of the cremasteric muscle and the vas deferens. The epididymal and scrotal types are less frequent and they originate from the smooth muscle surrounding the basement membrane of the epididymal canal and dartous layer, respectively [3]. Leiomyosarcomas have three typical histological features; these include perpendicularly arranged fascicles of spindle cells with eosinophilic cytoplasm, hyperchromatic blunt-ended nuclei, and scattered paranuclear vacuoles [4]. On immunohistochemical staining, expression of SMA, muscle specific actin, and desmin is observed in most leiomyosarcomas, while expression of CD34, myogenin, Ki-67, S-100 protein, and cytokeratin has also been reported in some cases [5]. This case showed a positive result for SMA, CD34, and desmin. Paratesticular leiomyosarcoma presents as a discrete nodular mass, which is completely separate from the testicle [2]. Although the etiology of leiomyosarcomas remains unclear, some authors have suggested local irradiation during childhood as a potential cause [6]. Clinically, most paratesticular leiomyosarcomas present as painless, slow-growing scrotal tumors in men of middle or older age. Occurrence of this disease is rare; therefore, the mode of spread is important. The most common means of spread is lymphatic, followed by hematogenous, and, last, by local extension. The route of lymphatic dissemination may involve the external iliac, hypogastric, common iliac, and para-aortic nodes. The lung is the primary site of blood-borne metastases. Local spread to the scrotum, inguinal canal, or pelvis along the pathway of the vas deferens is possible [3].
Paratesticular leiomyosarcoma is very rare and accumulation of a sufficient number of cases in order to document the natural history of such tumors along with treatment is difficult. Therefore, most documented treatments for paratesticular leiomyosarcoma have been categorized together with those for other paratesticular sarcomas. In general, the standard treatment for all paratesticular sarcomas consists of radical orchiectomy with high cord ligation. The role of additional systemic chemotherapy is not clear. However, paratesticular leiomyosarcoma has recently been classified according to the NCI system in order to determine the correlation between the tumor grade and clinical outcomes. According to one report, paratesticular leiomyosarcomas that were pathologic grade 1 and 2 (according to the NCI system) and that were treated with radical orchidectomy were free of recurrence and metastasis during the follow up period [5]. Although data from that report were insufficient, the importance of tumor grading for leiomyosarcoma in order to further assess the efficacy of various therapeutic options was demonstrated. Adjuvant therapy has not been well established, however, in earlier reports, adjuvant radiation therapy was usually recommended in order to reduce locoregional recurrence [7]. Although the role of adjuvant chemotherapy has not been fully established, some studies have reported on this. Findings of a meta-analysis of 14 randomized trials of sarcomas at various centers showed that doxorubicin-based adjuvant chemotherapy resulted in significant improvement of the time to local and distant failure, and, although it was not statically significant, a trend toward improved overall survival was observed [8]. In another study of adult sarcomas at different sites, doxorubicin based chemotherapy resulted in an increase in overall and metastasis free survival in patients with grade 3 sarcomas [9]. In our case, the tumor was NCI grade 3, and, after undergoing right orchiectomy, the patient received additional systemic chemotherapy using ifosfamide 1 g/m2 on days 1 to 3 plus adriamycin 30 mg/m2 on day 1 every three weeks. While undergoing systemic chemotherapy, the patient did not complain of any side effects and there was no bone marrow suppression, such as leukocytopenia. After nine cycles of systemic chemotherapy, the patient achieved a CR, and neither local recurrence nor distant metastases has occurred during the follow up period (12 months) after completion of systemic chemotherapy.
Due to the low number of reported cases of additional systemic chemotherapy for treatment of patients with stage III paratesticular leiomyosarcoma, the role of systemic chemotherapy has not been well established. And few domestic cases of paratesticular leiomyosarcoma have been reported [10-14], however, those cases were treatable with curative resection and the effect of chemotherapy against stage III paratesticular leiomyosarcoma was not documented, as in our case. In one retrospective analysis of the outcome of first-line chemotherapy in patients with male non-uterine advanced or metastatic leiomyosarcoma, median progression free and overall survival were 2.7 and 7.9 months, respectively [15]. As a result of successful treatment, this current case could be unique, and, although our case had a short-term follow up period of 12 months after systemic chemotherapy, 19 months disease free survival seems remarkable, compared with other cases. Longer term follow up is needed; therefore, the final results are still inconclusive.
In conclusion, this is a rare case of paratesticular leiomyosarcoma treated with orchiectomy and systemic chemotherapy. The role of chemotherapy in treatment of paratesticular leiomyosarcoma has not been well established, and this is still is a matter of discussion. However, this case has shown successful results with ifosfamide and adriamycin for treatment of stage III disease. Therefore, we report here on a case of paratesticular leiomyosarcoma treated successfully with orchiectomy and chemotherapy.