AbstractPurposeThe Korean National Cancer Screening Survey (KNCSS), a nationwide, annual cross-sectional survey, has been conducted since 2004. The current study was conducted in order to report on trends in cancer screening rates for five types of cancer (stomach, liver, colorectal, breast, and cervix uteri).
Materials and MethodsKNCSS data were collected between 2004 and 2012. The eligible study population included cancer-free men who were 40 years of age and older and women who were 30 years of age and older. The lifetime screening rate, screening rate with recommendation, and changes in annual rates were calculated.
ResultsLifetime screening rates and screening rates with recommendation for the five types of cancer rose steadily until 2010, showed a slight drop or were stable in 2011, and increased again in 2012. On average, screening rates with recommendation have shown annual increases of 4.3% (95% confidence interval [CI], 3.6 to 5.0%) for stomach cancer, 0.8% (95% CI, -0.5 to 2.1%) for liver cancer, 2.4% (95% CI, 1.3 to 3.5%) for colorectal cancer, 4.5% (95% CI, 3.9 to 5.1%) for breast cancer, and 1.3% (95% CI, 0.6 to 2.0%) for cervical cancer. Disparities in age groups and household incomes have been decreasing since 2004.
ConclusionCancer screening rates in Korea showed a significant increase from 2004 to 2012, and screening rates for gastric and breast cancer are now approaching 70%. The 10-Year Plan for Cancer Control target for screening rates was met or nearly met for all cancer types examined, with the exception of liver and colorectal cancer.
IntroductionIn Korea, cancer has ranked highest among all causes of death. During 2009, 69,780 cancer deaths were reported, accounting for 28% of all deaths. The cancer incidence rate for all sites combined showed an annual increase of 3.3% (1.6% in males, 5.3% in females) from 1999 to 2009 [1].
In an effort to reduce the burden of cancer, national cancer control programs were formulated by the Korean government in 1996, and the government established the National Cancer Screening Program (NCSP) in 1999. Since then, the target population and types of cancer covered have been expanded. Until 2001, the NCSP provided Medical Aid recipients with screening for three types of cancer (stomach, breast, and cervix); this service was provided free of charge. National Health Insurance (NHI) beneficiaries in the lower 20% income stratum were included in the NCSP in 2002. In 2003, NHI beneficiaries in the lower 30% income stratum and one additional type of cancer (liver) were included. In 2004, colorectal cancer was included in the NCSP, and, since 2005, the NCSP has provided Medical Aid recipients and NHI beneficiaries in the lower half of the income stratum with screenings for five types of cancer (stomach, liver, colorectal, breast, and cervix). NHI beneficiaries in the upper 50% income stratum receive screening services for the same five types of cancer from the NHI Corporation; however, they are required to pay 10% of the cost [2-6].
In addition to these organized cancer screening programs provided by the government, opportunistic cancer screening is widely available in Korea. Organized cancer screening programs utilize nationally implemented protocols that define a target population, screening interval, and follow-up strategies (Appendix 1). However, opportunistic cancer screening programs also include a variety of options in terms of the items screened, intervals between screening, and target cancer, depending on individual decisions or recommendations from health care providers. All costs of opportunistic cancer screening are paid entirely by users without a governmental subsidy. The current study was conducted in order to report on trends in overall cancer screening rates, including both organized and opportunistic cancer screenings among the Korean population.
Materials and MethodsThe Korean National Cancer Screening Survey (KNCSS), a nationwide, population-based, cross-sectional survey, has been conducted annually by the National Cancer Center since 2004. Stratified multistage random sampling based on resident registration population data is conducted according to geographic area, age, and gender. KNCSS data from 2004 to 2012 were used in this study. This study was approved by the Institutional Review Board of the National Cancer Center, Korea (approval no. NCCNCS-08-129).
According to the protocols of the NCSP (Appendix 1), people older than 40 years were eligible to undergo gastric cancer screening; those older than 50 years were included for colorectal cancer screening; women older than 40 years were eligible to undergo breast cancer screening; and women older than 30 years were included for cervical cancer screening. Screening for liver cancer was restricted to individuals older than 40 years, including those in high-risk groups, such as those who were positive for hepatitis B virus surface antigen or hepatitis C virus antibody or who had liver cirrhosis. The NCSP has provided screening for all members of the Korean population who are of the appropriate age. Therefore, the target population of this study was cancer-free men 40 years of age and older and women 30 years of age and older in each year.
For stratified multistage random sampling, the number of enumeration districts was designated in proportion to the population size by considering gender, age, and area, and the final study clusters were randomly selected. Five to eight households in an urban area and 10 to 12 households in a rural area were chosen randomly. The methods used for sampling were described in a previous study [7]. The data were collected by a professional research agency using face-to-face interviews, except in 2004, when the data were collected using computer-assisted telephone interviews. Subjects were recruited through door-to-door contact, and at least three attempts to contact each household were made. One person was selected from each household; if there was more than one eligible person in the household, the person whose date of birth was closest to the study date was selected. Informed consent was obtained from all study participants. Between 2005 and 2012, the response rates ranged between 34.5% and 58.5%.
Using a structured questionnaire, participants were asked about sociodemographic characteristics and their experience with screening for five types of cancer (stomach, liver, colorectal, breast, and cervix). The questions included: "Have you ever undergone [cancer type] screening?" and "Which screening method have you experienced?" For the interval between screenings, the question was: "When did you last undergo [cancer type] screening with this method?" To determine the reasons for undergoing screening or not undergoing screening, we asked: "What are your primary reasons for undergoing screening or not undergoing screening?" Distributions of sociodemographic characteristics of the study population for each year are shown in Appendix 2.
Two types of cancer screening rates were measured in this study. "Lifetime screening" was defined as having experienced each type of screening test. The "screening rate with recommendation" category was assigned to participants who had undergone screening tests according to the protocols of the NCSP (Appendix 1). However, for colorectal screening, respondents who underwent colonoscopy, double-contrast barium enema (DCBE), or fecal occult blood test (FOBT) within five, five, or one year, respectively, before 2009, and within 10, five, and one year, respectively, in 2009 and afterward were regarded as having undergone screening with recommendation.
Changes in annual lifetime screening rates and screening rates with recommendation were calculated as the annual percentage change (APC) within 95% confidence intervals (CIs) [8]. Screening rates were also calculated according to gender, age, and income. Monthly household income was subgrouped into three tertiles for each year. Due to an inadequate number of individuals within the high-risk group, as well as unstable results that showed a wide 95% CI, the liver cancer screening rate was excluded from subgroup analysis.
ResultsLifetime screening rates and screening rates with recommendation showed a continuous increase from 2004 until 2012. On average, between 2004 and 2012, the screening rate with recommendation showed an annual increase of 4.3% for gastric cancer, 0.8% for liver cancer, 2.4% for colorectal cancer, 4.5% for breast cancer, and 1.3% for cervical cancer (Table 1). Significant increasing trends were observed in the screening rates for gastric, colorectal, and breast cancer, but not in those for liver or cervical cancer. Despite a stable pattern, compared with 2010 and 2011, an increasing trend of screening rates was observed between 2004 and 2010 and between 2011 and 2012. Trends differed according to screening methods. The APC of the screening rate using upper endoscopy was more than twice the screening rate using upper gastrointestinal series (4.4% per year vs. 1.8% per year, respectively). On average, the colorectal cancer screening rate using FOBT showed a more rapid increase, compared with screening using colonoscopy or DCBE (3.0% per year vs. 1.9% per year, and 0.1% per year, respectively).
Among men, between 2009 and 2011, the screening rate with recommendation for stomach cancer showed a significant increase, while that of colorectal cancer showed a plateau (Fig. 1). In women, despite an increase in the rate of screening with recommendation for stomach and breast cancer, the trend for cervical and colorectal cancer uptake according to recommendations plateaued between 2009 and 2011. Screening rates for some types of cancer plateaued between 2009 and 2011; on the other hand, all cancer screening rates showed an increase in 2012, compared with those in 2011 in both men and women.
Overall screening rates with recommendation showed an increase in all age groups and for all types of cancer, with the exception of cervical cancer among women in their thirties (Fig. 2). The most significant increases were those of gastric cancer screenings and breast cancer screenings among subjects over the age of 70 years, both of which showed sharp increases when compared with other groups.
Screening rates with recommendation for stomach and breast cancer showed a steady increase at all income levels, and differences in screening rates showed a decrease among all income groups, compared with those in 2004 (Fig. 3). Screening rates for colorectal cancer peaked in 2008, and showed a decreasing pattern between 2008 and 2011, followed by an increasing pattern in all income groups. The screening rate for cervical cancer was lower in the low-income group than in the middle- and high-income groups, while gaps between groups showed a decrease. The most significant increases for cervical cancer screenings were in low-income women.
DiscussionLifetime screening rates and screening rates with recommendation for the five herein-described types of cancer have shown a significant increase since 2004. One of the goals of the second-term 10-Year Plan for Cancer Control, 2006-2015 [9] was achievement of an increase in cancer screening rates with recommendation to 70% by 2015. In this study, the screening rates with recommendation for stomach and breast cancer exceeded 70% in 2012. These rates achieved the target screening rate of the 10-Year Plan for Cancer Control. Screening rates for cervical cancer also came close to reaching that goal. However, screening rates for liver and colorectal cancer were low.
In the United Kingdom, where nationwide organized cancer screening has been implemented, 73.3% of women aged 45 to 74 years underwent mammography in 2009-2010 [10]. Differences in screening rates among age groups have shown a continuous decrease, and the screening rates for all age groups were over 70% in 2009-2010 [11]. The five-year coverage for cervical cancer screening using the Pap smear test has remained at 78.9% for women 25 to 49 years of age since 2008; however, in women 50 to 64 years of age, a slight decrease was observed, from 78.9% in 2009-2010 to 77.9% 2010-2011 [12].
In the United States, opportunistic cancer screening is superior to organized cancer screening [13]. The prevalence of having undergone recent screening with either FOBT or endoscopy was 46.8% in 2005 and 53.2% in 2008, indicating a 6.4% increase over the three-year period [14]. These rates were higher than those reported in Korea. In the United States, the screening rate using colonoscopy was much higher than that using FOBT, while in Korea, FOBT and colonoscopy showed similar total colorectal cancer screening rates. Home FOBT showed an increase until 2000 and then decreased through 2010. Colonoscopy showed an increase from 1987 to 1998, stabilized until 2000, and then began to rise again after 2000 and showed a particularly rapid increase (APC, 7%) from 2003 to 2010. In Korea, both the lifetime screening rate and screening rate with recommendation for colorectal cancer have shown a steady increase since 2004. In addition, the screening rate for colorectal cancer using FOBT showed a more rapid increase when compared with colonoscopy, which may be due to guidelines of the organized cancer screening program, which designated that only cases showing abnormal results on FOBT could undergo inspection by colonoscopy or DCBE.
Between 2000 and 2005, the screening rate showed a slight decline of 3.4% in the reported use of mammography in the past two years among women aged 40 years and older. Based on the National Health Interview Survey, the annual screening rate for breast cancer was 51% and 53% in 2005 and 2008, respectively, and declining trends were no longer apparent but instead rose overall and across groups for the recent period of 2005 through 2008 [15]. Screening rates for breast cancer of Korean women in the same year were lower than those reported; these rates have also risen steadily in Korea since 2004. In 2008, 78.3% of American women 18 years of age and older reported having undergone a Pap test within the past three years, indicating a small decrease of -1.3 percentage points (79.6% in 2005). The screening rate showed a slight increase until 2000, and then fell. As with breast cancer screening, no change in absolute differences in the rates of cervical cancer screening according to education was observed [16].
In Japan, the screening rate for gastric cancer was 11.8% in 2007, with a declining trend since the early 1990s [17]. The screening rate for colorectal cancer was 18.8%, trending toward a gradual increase (APC, 0.5%). The screening rate for breast cancer was 14.2%, trending toward a gradual increase. The screening rate for uterine cancer was 18.8%. These rates were lower than those reported in Korea.
Screening rates for colorectal, breast, and cervical cancer are slightly lower in Korea than in Western countries, such as the United States [14-16] and the United Kingdom [10-12]; however, they are higher than those in the average of member countries in the Organization for Economic Cooperation and Development (OECD) for breast cancer screening (62.2% in 2009) and cervical cancer screening (61.1% in 2009) [18,19].
This study has some limitations. The survey data were self-reported. Although survey-based results may be affected by recall bias, findings from many studies have demonstrated the reliability of self-reported histories of cancer screening, which have shown good agreement with medical records [20-22]. In addition, stratified multistage random sampling of survey data was performed according to geographic area, age, and gender, but not according to insurance type. In 2012, the proportion of Medical Aid recipients was low compared with that in other years. Because screening rates for Medical Aid recipients were lower than those for NHI beneficiaries (data not shown), the proportions of health insurance types may have affected the greater increase in screening rates in 2012. Finally, the response rate in our study ranged from 34.5% to 58.5%; however, compared with other nationwide studies conducted in Korea, in which response rates were less than 50% [23-25], our response rate can be considered acceptable.
Despite some limitations, this nationwide and population-based survey has been conducted annually since 2004. Therefore, the data were sufficiently representative for use in investigation of cancer screening rates, including both organized and opportunistic cancer screening, and the cancer screening rate showed a steady increase.
ConclusionScreening rates for five types of cancer have shown a steady increase since 2004, and those of some types of cancer reached the 10-Year Plan for Cancer Control target of 70%, excluding liver and colorectal cancer. Thus, the National Cancer Control Plan to reduce the economic burden of cancer has been implemented successfully; however, greater effort is still needed in order to increase the screening rates for liver and colorectal cancer.
AcknowledgmentsThis study was supported by a Grant-in-Aid for Cancer Research and Control from the National Cancer Center of Korea (no. 1010201).
References1. Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Seo HG, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2009. Cancer Res Treat. 2012;44:11–24. PMID: 22500156
2. Lee YY, Oh DK, Choi KS, Jung KW, Lee HY, Jun JK. The current status of gastric cancer screening in Korea: report on the National Cancer Screening Programme, 2009. Asian Pac J Cancer Prev. 2011;12:3495–3500. PMID: 22471504
3. Noh DK, Choi KS, Jun JK, Lee HY, Park EC. Factors associated with attending the National Cancer Screening Program for liver cancer in Korea. Asian Pac J Cancer Prev. 2012;13:731–736. PMID: 22524852
4. Shim JI, Kim Y, Han MA, Lee HY, Choi KS, Jun JK, et al. Results of colorectal cancer screening of the National Cancer Screening Program in Korea, 2008. Cancer Res Treat. 2010;42:191–198. PMID: 21253320
5. Oh DK, Shim JI, Han M, Kim Y, Lee HY, Jun JK, et al. Breast cancer screening in Korean women: report of the National Cancer Screening Program in 2008. J Breast Cancer. 2010;13:299–304.
6. Lee YH, Choi KS, Lee HY, Jun JK. Current status of the National Cancer Screening Program for cervical cancer in Korea, 2009. J Gynecol Oncol. 2012;23:16–21. PMID: 22355462
7. Lee HY, Park EC, Jun JK, Hahm MI, Jung KW, Kim Y, et al. Trends in socioeconomic disparities in organized and opportunistic gastric cancer screening in Korea (2005-2009). Cancer Epidemiol Biomarkers Prev. 2010;19:1919–1926. PMID: 20647409
8. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–351. PMID: 10649300
9. Han MA, Choi KS, Park JH, Moore MA, Park EC. Midcourse evaluation of the second-term 10-Year Plan for Cancer Control in Korea. Asian Pac J Cancer Prev. 2011;12:327–333. PMID: 21517281
10. NHS Cancer Screening ProgrammesNHS Breast Screening Programme: annual review 2011 [Internet]. Sheffield: NHS Cancer Screening Programmes; 2011. cited 2012 Dec 30Available from: http://www.cancerscreening.nhs.uk/breastscreen/publications/nhsbsp-annualre-view2011.pdf
11. The NHS Information CentreNHS Breast Screening Programme: annual review 2011 [Internet]. Sheffield: NHS Cancer Screening Programmes; 2011. cited 2012 Dec 30Available from: http://www.cancerscreening.nhs.uk/breastscreen/breast-statistics-bulletin-2009-10.pdf
12. NHS Cancer Screening ProgrammesNHS Cervical Screening Programme: annual review 2011 [Internet]. Sheffield: NHS Cancer Screening Programmes; 2011. cited 2012 Dec 30Available from: http://www.cancerscreening.nhs.uk/cervical/publications/cervical-annual-review-2011.pdf
13. Smith RA, Cokkinides V, Brooks D, Saslow D, Shah M, Brawley OW. Cancer screening in the United States, 2011: a review of current American Cancer Society guidelines and issues in cancer screening. CA Cancer J Clin. 2011;61:8–30. PMID: 21205832
14. National Cancer InstituteCancer trends progress report: 2011/2012 update. Colorectal cancer screening [Internet]. Bethesda, MD: National Cancer Institute; 2012. cited 2012 Dec 30Available from: http://progressreport.cancer.gov/doc_detail.asp?pid=1&did=2009&chid=92&coid=918&mid=
15. National Cancer InstituteCancer trends progress report: 2011/2012 update. Breast cancer screening [Internet]. Bethesda, MD: National Cancer Institute; 2012. cited 2012 Dec 30Available from: http://progressreport.cancer.gov/doc_detail.asp?pid=1&did=2009&chid=92&coid=916&mid=#trends
16. National Cancer InstituteCancer trends progress report: 2011/2012 update. Cervical cancer screening [Internet]. Bethesda, MD: National Cancer Institute; 2012. cited 2012 Dec 30Available from: http://progressreport.cancer.gov/doc_detail.asp?pid=1&did=2009&chid=92&coid=917&mid=#trends
17. Yoshida M, Kondo K, Tada T. The relation between the cancer screening rate and the cancer mortality rate in Japan. J Med Invest. 2010;57:251–259. PMID: 20847525
18. OECDHealth at a glance 2009: OECD indicators. Screening, survival and mortality for cervical cancer [Internet]. OECD iLibrary; 2011. cited 2012 Dec 30Available from: http://www.oecd-ilibrary.org/docserver/download/8109111ec054.pdf?expires=1356786645&id=id&accname=guest&checksum=1686480C1DB188423551F0E89AC80D67
19. OECDHealth at a galance 2009: OECD indicators. Screening, survival and mortality for breast cancer [Internet]. OECD iLibrary; 2011. cited 2012 Dec 30Available from: http://www.oecdilibrary.org/docserver/download/8109111ec055.pdf?expires=1356786924&id=id&accname=guest&checksum=2AD9534B55A7A6B54E7BCFF5F8C467F5
20. Caplan LS, McQueen DV, Qualters JR, Leff M, Garrett C, Calonge N. Validity of women's self-reports of cancer screening test utilization in a managed care population. Cancer Epidemiol Biomarkers Prev. 2003;12(11 Pt 1):1182–1187. PMID: 14652278
21. Hoffmeister M, Chang-Claude J, Brenner H. Validity of self-reported endoscopies of the large bowel and implications for estimates of colorectal cancer risk. Am J Epidemiol. 2007;166:130–136. PMID: 17456475
22. Jones RM, Mongin SJ, Lazovich D, Church TR, Yeazel MW. Validity of four self-reported colorectal cancer screening modalities in a general population: differences over time and by intervention assignment. Cancer Epidemiol Biomarkers Prev. 2008;17:777–784. PMID: 18381476
23. Ock SM, Choi JY, Cha YS, Lee J, Chun MS, Huh CH, et al. The use of complementary and alternative medicine in a general population in South Korea: results from a national survey in 2006. J Korean Med Sci. 2009;24:1–6. PMID: 19270805
24. Park B, Lee YK, Cho LY, Go UY, Yang JJ, Ma SH, et al. Estimation of nationwide vaccination coverage and comparison of interview and telephone survey methodology for estimating vaccination status. J Korean Med Sci. 2011;26:711–719. PMID: 21655054
25. Seo HJ, Sung YK, Choi CB, Lee EB, Cheong C, Kim SY, et al. Prevalence and factors affecting glucosamine use in Korea: a survey-based study. Rheumatol Int. 2013;33:1627–1631. PMID: 22200808
AppendicesAppendix 1Cancer screening protocols issued by the National Cancer Screening Program (NCSP) in Korea
UGI, upper gastrointestinal series; AFP, alpha-fetoprotein; FOBT, fecal occult blood test. a)In the case of an abnormality on the UGI, endoscopy is recommended, and a biopsy is performed when an abnormality is found during endoscopy, b)Patients at high risk for liver cancer include those with chronic hepatitis determined from serological evidence of infection with hepatitis B or C virus or liver cirrhosis, c)In the case of an abnormality on FOBT, colonoscopy or a double-contrast barium enema is recommended, and a biopsy is performed when an abnormality is found during colonoscopy.
Appendix 2Distribution (%) of sociodemographic characteristics of the study population in the Korean National Cancer Screening Survey (KNCSS), 2004-2012
a)Restricted to women aged 30-39 years, b)Due to missing data, some row sums are not 100% every year, c)1 USD=1,000 KRW, d)Others: divorced or separated, e)The question related to residential area did not distinguish between urban and rural areas in 2004.
Fig. 3Cancer screening rates with recommendation by household income level, 2004-2012. Monthly household income status classified by tertile. 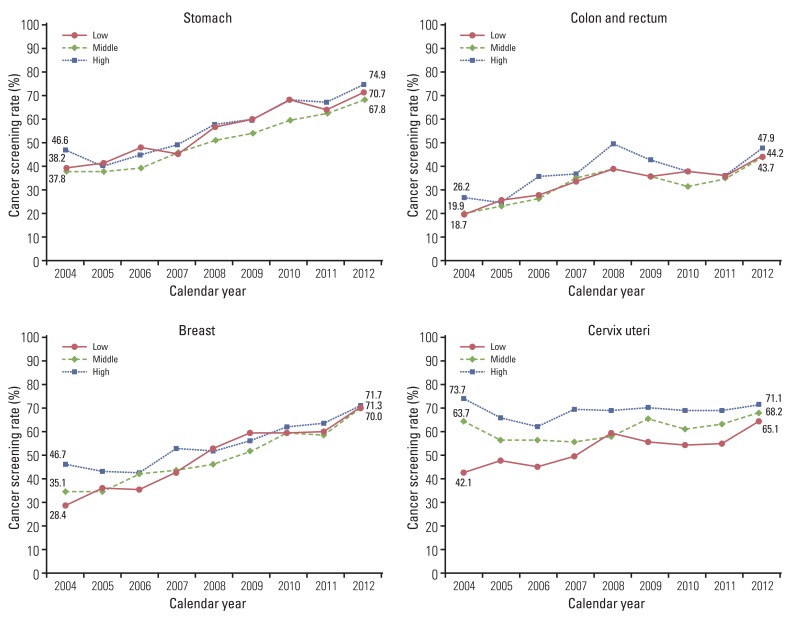
Table 1Cancer screening rates for five major cancers in Korea, 2004-2012
APC, annual percent change; CI, confidence interval; UGI, upper gastrointestinal; DCBE, double-contrast barium enema; FOBT, fecal occult blood test. a)Lifetime screening rate was defined as the proportion of respondents who ever underwent the screening test(s), b)Screening rate with recommendation was defined as the proportion of respondents who fulfilled the screening recommendation criteria among the respondents in the targeted age group for the relevant cancer, c)Respondents were restricted to men and women who were 40 years old and over who had last undergone upper endoscopy or UGI series screening within a period of two years, d)Respondents were restricted to men and women who were 40 years old and over who were at high risk for liver cancer [hepatitis B virus surface antigen (+), hepatitis C virus antibody (+), or liver cirrhosis] who had last undergone screening with abdominal ultrasonography and serum alpha-fetoprotein within a period of six months, e)Respondents were restricted to men and women who were 50 years old and over who had last undergone screening with colonoscopy, DCBE, or FOBT within a period of 10, five, or one years, respectively. However, before 2009, patients who underwent colonoscopy within a period of five years were regarded as having undergone screening with recommendation, f)Respondents were restricted to women who were 40 years old and over who had last undergone screening with mammography within a period of two years, g)Respondents were restricted to women who were 30 years old and over who had last undergone screening with conventional cytology within a period of two years. |
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||