INTRODUCTION
Brainstem tumors constitute at least 10% of all childhood brain tumors (1). The majority of brainstem gliomas are diffuse on imaging, originate in the pons and extend toward other portions of the brainstem (2). There is overall agreement that surgery plays little role in patients with these tumors, and radiation therapy is the mainstay of treatment with a palliative intent, because the 3-year survival rate of children diagnosed with a diffuse brainstem glioma, treated with radiotherapy and/or chemotherapy, is still only 5 to 15%. Several experimental studies aimed at delivering more intensive therapy have been tested. Hyperfractionated radiation therapy and brachytherapy have been used for this purpose, and produced no meaningful change in the results (3~6). Several chemotherapeutic studies, using myeloablative doses of chemotherapy, and hormonal therapy have been unable to demonstrate better outcomes (7~11). The purpose of this study was to evaluate the outcome and prognostic factors in patients with a diffuse childhood brainstem glioma following radiation therapy.
MATERIALS AND METHODS
1) Patient characteristics
Between June 1986 and August 2001, 50 consecutive patients with a newly diagnosed brainstem glioma were treated with radiation therapy at the Department of Radiation Oncology, Seoul National University Hospital. Among these patients, five with an exophytic tumor, treated with surgery and expected to have a better prognosis, were excluded from this analysis. The diagnosis of diffuse brainstem glioma was based on the following clinical and radiological criteria: (1) duration of signs and symptoms of less than 6 months; (2) the presence of one of the followings: pyramidal tract involvement, cerebellar ataxia or cranial nerve deficit attributable to the tumor; (3) cranial magnetic resonance imaging (MRI) on diagnosis showing diffuse involvement of the brainstem. Histological confirmation was achieved in 13 of the 45 patients. The patient characteristics are summarized in Table 1.
2) Radiation therapy
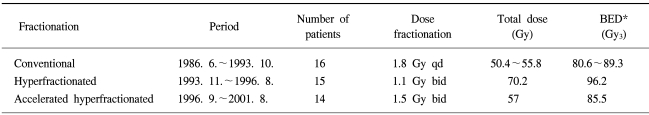
All patients were treated with 4MV photon beam radiation therapy through parallel opposed lateral fields. The planned target volume encompassed the entire gross tumor volume, as determined by the T2-weighted hyperintense signal on MRI, plus a 2 cm margin in all directions. The dose fractionation schedules differed according to the period (Table 2). Between 1986 and 1993, conventional fractionation for the radiation therapy, comprising of 1.8 Gy once a day, 5 days a week, for a total dose 50.4 to 55.8 Gy was used. Between 1993 and 1996, a hyperfractionated schedule of 1.1 Gy twice a day, at least 6 hours apart, 5 days a week, for total dose up to 70.2 Gy was employed. After 1996, an accelerated hyperfractionated schedule of 1.5 Gy twice a day, at least 6 hours apart, 5 day a week, for a total dose up to 57 Gy has been adopted. In 13 patients with confirmed pathology, two were irradiated with conventional fractionation, two with hyperfractionated schedule, and nine were treated with accelerated hyperfractionated radiation therapy. All patients received steroid medication before and during the radiation therapy.
3) Adjuvant chemotherapy
Between October 1996 and November 1998, nine patients who finished their radiation therapy were treated with adjuvant treatment. Six patients received chemotherapy, the 8 in 1 (vincristine, hydroxyurea, procarbazine, CCNU, cisplatin, cytosine arabinoside, high-dose methylprednisolone, and cyclophosphamide), CCG 9931 (vincristine, etoposide, cisplatin, cyclophosphamide alternating with carboplatin and etoposide) and CCG 9921 (vincristine, cisplatin, cyclophosphamide, etoposide) regimens in one patient each, and the other three patients received chemotherapy with the CCG 9941B regimen (cisplatin, etoposide, cyclophosphamide, vincristine) as adjuvant treatment. Three patients also received adjuvant hormonal therapy using tamoxifen.
4) Statistical analysis
The overall survival was defined as the time interval from the start of radiation therapy to death from any cause or to the date of the last follow up evaluation. The progression free survival was assessed from the date of radiation therapy to the date of disease progression, as constituted by a clinical neurologic and/or radiological change or death, whichever came first. The overall survival and progression free survival were calculated using the Kaplan-Meier method (12). The differences between the curves were compared by the log-rank test (13). The SAS system v.8.0 (SAS Institute Inc. Cary, NC.) was used for data processing.
RESULTS
1) Response to treatment
After radiation therapy, neurologic improvements were seen in 42 of the 45 patients (93%), but the other 3 showed no clinical improvement.
The radiological response documented 4 to 8 weeks subsequent to the completion of radiation therapy was used as the objective radiological response. These responses were assigned to one of the following categories: (1) complete response, marking the complete disappearance of all measurable tumor, with simultaneous neurological improvement; (2) partial response, defined as a shrinkage of 50% or more in volume of all measurable lesions, with simultaneous neurological improvement; (3) minimal response, indicating a tumor shrinkage between 25 and 50%, without neurological deterioration; (4) stable disease, defined as a tumor shrinkage of less than 25%, without neurological deterioration and (5) progressive disease, defined as a 25% or more increase in the tumor volume or the presence of new lesions, with simultaneous neurological deterioration.
Of the 45 patients, 39 were assessable for an objective radiological response, 6 refused radiological examination due to disease progression or economic problems (3 patients each). Among the 39 assessable patients, 22 (56%) had a partial response; 13 (33%) a minimal response; three (8%) a stable disease; and one (3%) a progressive disease.
Of the 9 patients treated with adjuvant treatment, 6 revealed a partial response and 3 showed a progressive disease, radiologically.
2) Survival
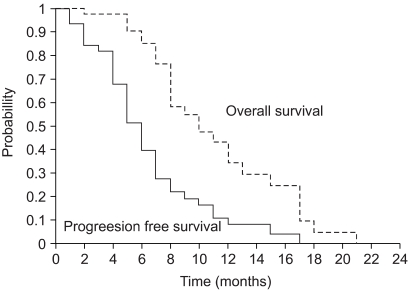
The median survival time was 12 months. The 1-year overall survival and progression free survival rates and median progression free survival time were 41 and 14%, and 7 months, respectively (Fig. 1).
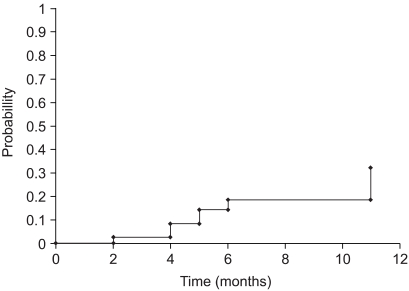
Leptomeningeal metastases were observed in seven patients (16%) by MRI. The 1-year actuarial rate of leptomeningeal metastasis was 32% (Fig. 2). Four patients with leptomeningeal seeding had a stable disease at the primary site, and 3 had leptomeningeal metastases, with a progressive disease at the primary site. In these 7 patients, the pathology was known for 5. Four and 1 patient had high and low grade histologies, respectively. There were no differences in the survival between the patients who showed leptomeningeal seeding and those without.
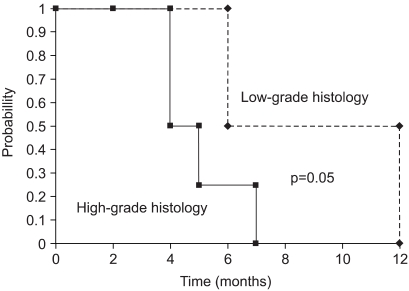
As prognostic factors, no variable was found to have significance on the overall survival. There was no difference in the survival between the different fractionation schedule groups. Thirteen patients had a pathologically confirmed disease, and in these patients, the tumor histology (low-grade vs. high-grade) was a statistically significant prognostic factor for progression free survival (p=0.05, Fig. 3). However, the number of patients was too small, with all eventually showing a dismal prognosis; therefore, the true significance of this variable was not evident.
3) Toxicity
Otitis media developed in five patients (11%) and steroid dependency (prolonged use of more than 3 months after completion of radiation therapy) occurred in 15 (33%), of whom 8 were in the hyperfractionated and 4 in the accelerated hyperfractionated radiation therapy groups. On follow up MRI, intralesional necrosis was found in one patient (2%).
DISCUSSION
Brainstem glioma remains a therapeutic dilemma. Because of the location of these lesions, aggressive surgery is contraindicated. Unfortunately, radiation therapy alone, or combined with chemotherapy, has been fraught with poor survival outcomes (7~10).
Trials using hyperfractionated radiation therapy have been the main focus of clinical research over the past years. The intent of hyperfractionated radiation therapy is the reduction of the late effects to normal tissue (such as normal brain) and the achievement of the same or a better tumor control as the dose per fraction is decreased (14). Theoretically, such sparing of the dose limiting normal tissue should allow for higher total doses to the tumor, without increasing untoward toxicity, resulting in an improved therapeutic index. Because a dose response relationship has been observed for malignant gliomas and autopsy data implies that the cause of failure is a locally progressive disease, and a higher total tumor doses should results in higher local control rates, with subsequently improved survival outcomes (15,16). However, trials using hyperfractionated radiation therapy, in combination with chemotherapy, failed to improve the outcomes, but so far have increased the toxicity; therefore, conventional radiation therapy, using a total dose of 54 Gy in 1.8 Gy daily fractions is recommended for the treatment of diffuse brainstem gliomas (3~5).
In our study, hyperfractionated and accelerated hyperfractionated radiation therapy showed no statistically significant survival advantage, but hyperfractionated radiation therapy showed higher steroid dependency. Now, our institution uses a conventional fractionation schedule of 54 Gy in 1.8 Gy daily fractions as a standard treatment protocol.
Leptomeningeal metastases were observed in 7/45 patients (16%) and the actuarial 1-year rate of leptomeningeal seeding was 32% in this study. In a Pediatric Oncology Group Study, the rate of leptomeningeal metastasis was similar to that found in our study; 6 out of 39 patients (15%) (17). Interestingly, among these patients, 5 underwent stereotactic biopsy for pathologic confirmation. It might be presumed that the biopsy procedure effected leptomeningeal seeding, but the number of patients was too small to confirm the relationship between the biopsy procedure and leptomeningeal seeding.
In 13 patients with a confirmed pathology, a low grade tumor histology was the only favorable factor of progression free survival in this group (p=0.05). The role of stereotactic biopsies for diffuse brain stem lesions in children is controversial. Some authors state that MRI should replace biopsies in children with diffuse brainstem tumors. It may be dangerous and might not reveal the real tumor grade (18). Others disagree with this view, as they have found a good correlation between the histological grade and clinical course. Cartmill and Punt described the results from 18 children who underwent a stereotactic biopsy of their brainstem lesions. In their report, children with low-grade gliomas had better outcomes than those with higher grade lesions (19). For diagnostic purposes, MRI has now superseded the need for a stereotactic biopsy. Should a treatment be developed that is more effective, a biopsy may also help to direct an appropriate therapy (20). A recent study, analyzing 28 brainstem gliomas, demonstrated a correlation between the tumor grade and EGFR (Epidermal Growth Factor Receptor) protein expression. There is considerable evidence that inhibitors of ERBB1 tyrosine kinase might have therapeutic efficacy against high-grade gliomas (21). Some in vitro and in vivo studies, using ZD1839 (Iressa), an inhibitor of the EGFR (ERBB1) tyrosine kinase, for a brain tumor cell line or brain tumor patients, including brainstem glioma were recently published, which showed optimistic results (22,23). The PBTC (Pediatric Brain Tumor Consortium) in the United States recently commenced a Phase I/II study of Iressa in children with high-grade supratentorial astrocytoma and nondisseminated diffuse intrinsic brainstem gliomas. It is hoped that a more effective treatment method can be provided from that study.
CONCLUSIONS
The survival of brainstem glioma patients was not influenced by the radiation therapy fractionation schedule, but was dependent upon the tumor histology. Because all the previous efforts to improve outcomes for patients with diffuse brainstem gliomas achieved no significant gains, more aggressive treatments, including targeted therapy, should be investigated.