AbstractIntroduction of the concept for oligometastasis led to wide application of metastasis-directed local ablative therapies for metastatic colorectal cancer (CRC). By application of the metastasis-directed local ablative therapies including surgical resection, radiofrequency ablation (RFA), and stereotactic ablative body radiotherapy (SABR), the survival outcomes of patients with metastatic CRC have improved. The liver is the most common distant metastatic site in CRC patients, and recently various metastasis-directed local therapies for hepatic oligometastasis from CRC (HOCRC) are widely used. Surgical resection is the first line of metastatic-directed local therapy for HOCRC, but its eligibility is very limited. Alternatively, RFA can be applied to patients who are ineligible for surgical resection of liver metastasis. However, there are some limitations such as inferior local control (LC) compared with surgical resection and technical feasibility based on location, size, and visibility on ultrasonography of the liver metastasis. Recent advances in radiation therapy technology have led to an increase in the use of SABR for liver tumors. SABR is considered complementary to RFA for patients with HOCRC who are ineligible for RFA. Furthermore, SABR can potentially result in better LC for liver metastases > 2–3 cm compared with RFA. In this article, the previous studies regarding curative metastasis-directed local therapies for HOCRC based on the radiation oncologist’s and surgeon’s perspective are reviewed and discussed. In addition, future perspectives regarding SABR in the treatment of HOCRC are suggested.
IntroductionOligometastasis (OM) was suggested by Hellman and Weichselbaum in 1995 [1] as a disease status in which the facility for metastatic growth is not fully developed and the numbers of metastases and the affected organ sites are limited. Hellman’s suggestion was based on the evidence showing that ablative local therapies for metastasis from various primary tumors resulted in extended survival or even curation in some patients [1–5]. After the introduction of this concept, the roles of metastasis-directed ablative local therapies of metastases from various primary tumors have been evaluated in numerous studies showing the benefits of metastasis-directed ablative local therapies in the improvement of survival outcomes [6–8]. However, the definitions and criteria of OM are diverse among the studies, especially in the number of metastases or affected organ sites, and has not been standardized, yet [9,10]. Therefore, the efforts to achieve the consensus have been made among the clinicians [11,12]. In the development of OM concept, data from early studies dealing with colorectal cancer (CRC) were utilized as evidence and current strategies recommended in the treatment of metastatic CRC (mCRC) depend on this concept [3,4].
It was reported that, in 2020, CRC accounted for 10% of the global cancer incidence, which was ranked in the third place following breast cancer and lung cancer and 9.4% of all cancer deaths, which was ranked in the second place following lung cancer [13]. Among the patients with CRC, 22% have initially diagnosed as stage IV CRC [14]. While the rates of distant metastasis in patients with stage I–II CRC are as low as at most 20%, 25%–50% of stage III patients may experience distant metastasis (including lymph node metastasis) later, which could be reduced in the range of 25%–30% following complete surgical resection plus subsequent adjuvant chemotherapy [15]. Although the survival time for patients with mCRC has been significantly extended over time, the reported 5-year overall survival (OS) rate remained < 20% [16]. The advances in various treatment strategies, including systemic therapy and local treatment for primary and metastatic disease, have contributed to the increased survival outcomes in the patients with mCRC. Especially, after the introduction of OM concept, metastasis-directed local ablative therapies have widely been utilized for hepatic or lung metastasis and resulted in the improved outcomes through successful local control (LC).
The liver is the most common site of distant metastasis in the CRC patients, which is related with the portal circulation, and accounts for approximately 25%–30% [17,18]. Although systemic treatment has played a critical role in metastatic setting, surgical resection of hepatic OM from CRC (HOCRC) has been recommended for the selected resectable cases which resulted in the improved 5-year OS rates upto 47%–60% [19–21]. However, only 15%–25% of HOCRC patients are eligible for resection due to the tumor or patient factors [22,23]. Therefore, alternative local ablative therapies were required to treat the HOCRC patients who are unsuitable for surgical resection. In the current guidelines for mCRC, various liver metastasis-directed local ablative therapies other than resection are listed that include radiofrequency ablation (RFA), microwave ablation (MWA), stereotactic ablative body radiotherapy (SABR), and embolization techniques [5,24].
Liver-directed local radiation therapy (RT) used to be regarded as unsafe, in the past, due to the fear of the risk for radiation-induced liver disease (RILD). Recent advances in RT technology during the last decade, however, have enabled highly precise and accurate liver-directed high-dose irradiation, and extended the use of new RT techniques in treating the HOCRC patients. In the previous prospective studies, the outcomes following SABR for liver metastasis from various primary sites showed high 2-year LC rate over 90% [25,26]. Furthermore, in the recent trials, SABR has improved the survival outcomes when compared with the standard of care for OM from various primary cancers, and the use of SABR for ablation of HOCRC is expected to increase. No randomized controlled trial comparing SABR with other modalities, however, has been performed yet, and the optimal regimen of SABR for HOCRC needs to be established.
Herein, the literature regarding curative local therapies for HOCRC is reviewed, and the role of SABR is discussed from the radiation oncologist’s and surgeon’s perspective. In addition, the future potential of SABR for treating the HOCRC patients is suggested.
Surgical Resection of HOCRCHistorically, curative resection was first attempted in the 1900s, and the relevant results from small series were reported. However, in the 1980s, a large amount of data from 24 institutions was published by Hughes et al. [3], which reported that curative resection in 607 HOCRC patients resulted in a 5-year disease-free survival (DFS) rate of 25%. These data supported the Hellman’s suggestion for the OM concept together with other series regarding pulmonary metastasectomy in sarcoma and renal cell cancer patients [1]. Subsequent large series on HOCRC endorsed the initial publication [27]. In a multicenter study by Pawlik et al. [28], a significantly improved 5-year OS rate of 58% was reported, when compared with the previous study. In particular, the researchers reported a significant association of negative resection margin with improved survival rate [28]. Recently, Bogach et al. [29] evaluated the outcome of resection of HOCRC at the population level, including 1,168 patients in the province of Ontario, Canada, from 2006 to 2015. They reported that the proportion of the patients who underwent resection increased 3% per year on average, and staged resection was more frequent than simultaneous resection (62% vs. 38%). The 5-year OS rate was 48% in the total population, and those who underwent simultaneous resection, when compared with staged resection patients, were associated significantly with shorter hospital stay (8 days vs. 11 days, p < 0.001), less frequent major resection (17% vs. 65%, p < 0.001), higher 90-day mortality (6% vs. 1%, p < 0.001), shorter median survival (40 months vs. 78 months, p < 0.001), and lower OS rate at 5 years (37.2% vs. 54.8%, p < 0.001), respectively. In various studies, long-term survival was also consistently reported. In Table 1, the relevant information of the selected studies is summarized. The improved OS rates following resection of HOCRC were not the only important findings in these studies. Various prognostic factors, including the number of hepatic tumors, size of hepatic metastasis, margin status after hepatic resection, disease-free interval, extrahepatic disease, disease burden of primary tumor, and tumor marker level, were also identified [30,31]. These parameters formed the basis of the OM concept, which were considered in the criteria and goals of resection of HOCRC. However, the consensus and eligibility criteria for resection of HOCRC have not established yet. Specifically, because the eligibility for surgical resection mainly depends on the estimated remnant liver volume following resection, underlying liver functional status, and location of metastatic tumor, only a small portion of the HOCRC patients is amenable to this approach. The surgical resection, however, has been extended along with a few new approaches: conversion therapy, which can shrink the tumor size and potentially convert from unresectable to resectable status; extending resection to extrahepatic disease; two-stage hepatectomy; and portal vein embolization inducing hypertrophy of the future liver remnant. Furthermore, the outcome of surgical resection of HOCRC could be improved by perioperative administration of chemotherapy [32]. However, there is a high percentage of HOCRC patients in whom complete LC could be attempted but surgery is not regarded a viable option. Therefore, alternative and supplementary methods to surgical resection are required, which include RFA, MWA, and SABR.
Radiofrequency Ablation for Hepatic OligometastasisRFA is the most commonly used local ablative approach. RFA can be conducted percutaneously or intraoperatively by placing the ablation electrodes in or around the tumor creating a thermal necrosis zone within the tumor and adjacent area [35]. RFA has shown up to 95% tumor response rates and safety in selected HOCRC patients who are not candidates for surgical resection [35,36].
Following RFA, excellent LC rate has been reported. In a randomized controlled trial, aggressive local treatments using RFA with or without surgical resection in addition to systemic treatment resulted in prolonged OS when compared with systemic treatment alone [37], which has made RFA a valid local ablative modality for HOCRC. However, when compared with surgical resection, RFA showed inferior outcomes. In a prospective randomized controlled trial, in the HOCRC patients with low tumor burdens and amenability to surgery, the outcomes following RFA and surgical resection, as the first-line treatment, were compared. This trial reported the local recurrence rates of 32% and 4% at the site of ablation and resection, respectively (p < 0.001) [38]. Several previous studies compared RFA and surgical resection (Table 2), which showed generally inferior LC and OS rates following RFA [27–36]. Kron et al. [39] performed a systematic review of 18 published studies and reported that among the studies, 10 and eight showed significantly higher local recurrence rates and lower OS and DFS rates in the RFA group than in the surgical resection group, respectively. These trends of higher local recurrence and lower OS and DFS rates in the RFA group were maintained for technically resectable or even solitary liver metastasis from CRC. Similarly, a meta-analysis of 26 studies regarding microwave, RFA and surgical resection for liver metastasis from CRC showed that the risk of hepatic recurrence was significantly higher with odd ratio (OR) of 3.94 (p < 0.001) in RFA group comparing with surgical resection group [40]. The OS and DFS at 5 years were also favored surgical resection rather than RFA with hazard ratios (HR) of 1.30 (p=0.003) and 1.40 (p < 0.001) [40]. Especially, the risk of local recurrence was significant higher in subgroups of tumor size of 3 cm or less (OR, 7.26; p < 0.001) and solitary HOCRC (OR, 7.13; p < 0.001) for RFA comparing with surgical resection. The 5-year OS of solitary HOCRC subgroup was significantly superior in surgical resection group comparing with RFA (HR, 1.77; p=0.008) [40]. Therefore, RFA is not sufficient to be compatible with surgical resection as a standard treatment for HOCRC. Various reasons have been proposed to explain the inferiority of RFA. One suggested that resection might remove the occult hepatic micrometastases, which could not be adequately ablated by RFA [39]. Another suggestion was the potential selection bias in the studies in which the patients receiving RFA could have had poorer biological characteristics related to ineligibility for surgery [41].
Despite the inferior outcomes, RFA still remains a valuable option for the HOCRC patients who are ineligible for surgical resection. In addition, neither conclusive results nor established criteria for the modality choice have made through any randomized controlled trial so far. There are ongoing randomized trials comparing RFA with surgical resection including COLLISION trial (NCT03088150), HEL-ARC trial (NCT02886104), and LAVA trial (ISRCTN52040363). COLLISION trial is enrolling the CRC patients with 1–10 liver metastases (size ≤ 3 cm) and no extrahepatic metastasis eligible to both surgical resection and thermal ablation in the Netherlands [51]. HELARC trial, which is being conducted in China, aims to compare the surgical resection and thermal ablation in the CRC patients with 1–3 liver metastases (size ≤ 3 cm) and no extrahepatic metastasis who are suitable to both modalities [52]. In LAVA trial, which is conducted in the United Kingdom and the Netherlands, enrolls high-risk CRC patients with liver metastases who have poor prognostic factors (e.g., poor response after chemotherapy, curable extrahepatic disease, or multiple synchronous metastasis, etc.), and the requirement of high-risk surgery such as staged hepatectomy with or without portal vein ligation or embolization [53]. These trials are expected to provide informative results and to aid in establishing the useful criteria for modality choice.
SABR for Hepatic OligometastasisSABR is a widely used RT modality for local ablation of both primary and metastatic tumors leading to the LC rates over 90%. Recently, use of SABR for treatment of OM from various malignancies is expected to increase, based on validation through the SABR-COMET trial, which showed the superiority of SABR compared with standard of care [8]. SABR has also consistently shown excellent LC rates for HOCRC (Table 3), however, there are limited number of studies that evaluated the efficacy of SABR exclusively for the HOCRC patients.
The characteristics of the study population were diverse, including tumor factors, and thus, the reported outcomes were quite heterogeneous. A few certain factors in the patients’ characteristics or treatment parameters, however, consistently showed a significant association with the oncological outcomes in the previous reports. The tumor size was an important independent factor associated with the oncological outcomes. Doi et al. [59] showed tumor size ≥ 30 mm was a significant independent risk factor for low LC rate with HR of 3.940 (p=0.0314). McPartlin et al. [57] reported the sum of gross tumor volume and the presence of extrahepatic disease at the time of SABR as the independent factors for OS (HR, 1.27; p=0.017 and HR, 2.11; p=0.005, respectively). In addition to the tumor factors, the prescribed dose was a critical factor for LC. Joo et al. [58] reported that the 2-year LC rates significantly differed based on the prescribed biologically effective dose (with α/β ratio of 10) of ≤ 80 Gy, 100–112 Gy, and ≥ 132 Gy (52%, 83%, and 89%, respectively). In another study, increasing the minimum dose relative to the gross tumor volume was associated with the improved LC rate of 41% at 4 years in the patients receiving dose ≥ 37.6 Gy when compared with 0% for the others [57]. These results indicated that the candidates with small-sized liver metastasis, low burden of total liver metastasis, absence or control of extrahepatic disease, and higher radiation dose should serve as the selection criteria for SABR to achieve satisfactory LC rates.
SABR has often been compared with RFA for hepatic malignancy, especially, hepatocellular carcinoma (HCC) [41–43]. Because both modalities are non-surgical approaches, the indications of each modality overlap but not the same. Therefore, the choice between these modalities should not be randomly made [60]. RFA is not applicable to the tumors located in the invisible area by ultrasonography, such as the subphrenic area or an area where the probe cannot be properly approached [61]. RFA is also unsuitable for the tumors proximal to the vasculature due to the potential heat sink effect that can reduce the ablation volume and mitigate the LC rate [62]. Furthermore, despite the low complications rates, RFA has the potential to cause procedure-related issues including hepatic bleeding, pleural effusion, biliary fistula, skin burn, pneumothorax, peritoneal seeding, and pleural hemorrhage. Thus, the patients at risk of these complications are not the appropriate candidates of RFA [63,64]. Conversely, the anatomical limitations appear to be less significant issue and seldom relevant in SABR when compared with RFA [65]. Hepatotoxicity and bowel damage adjacent to the target volume, however, are the concerns with the liver-directed SABR [65]. The risk of hepatotoxicity following SABR is associated with radiation dose, irradiated volume, and underlying liver function. The risk of bowel damage depends on the proximity of the target volume to the corresponding bowel. Although the rates of relevant toxicities were reported as < 1% following SABR, proper patient selection considering patient- or tumor-related factors is highly required [63].
No randomized controlled trial that compared both modalities for local ablation of any hepatic malignancy has been reported yet. Though a phase III randomized trial of SABR vs. RFA for HOCRC with one-to-four inoperable hepatic metastases (RAS01, NCT01233544) was initiated by a Danish group, it was terminated early due to the insufficient patients’ recruitment [66]. Currently, there is no ongoing clinical trial of the relevant issue [60]. There are several retrospective studies that compared two modalities [50–55], which generally showed similar LC rates (Table 4). Furthermore, in subgroup analysis, LC rates following SABR for primary HCC or hepatic metastasis > 2 cm tended to be better when compared with RFA. In various studies, as the tumor size increased, the difference in the LC rates was greater following RFA when compared with SBRT. Yu et al. [67] compared RFA and SABR for treatment of HOCRC. They performed subgroup analysis by adjustment with the inverse probability of treatment weighting and showed that SABR resulted in significantly higher LC rate (HR, 0.153; p < 0.001) in the patients’ subgroup with tumor size > 2 cm, while not in the subgroup of tumor size ≤ 2 cm (HR, 0.648; p=0.10), respectively [67]. Similarly, Franzese et al. [68] showed significantly higher LC rate following SABR (91%) when compared with ablative therapy using MWA (84%) in the subgroup of liver metastasis from CRC (p=0.0214), and in the subgroup with tumor size ≥ 3 cm, the discrimination between the modalities were much larger (p=0.005) than in the subgroup with tumor size < 3 cm (p=0.238), indicating that SABR was a better modality for tumor size > 2 cm when compared to RFA. Considering the risk of complications in the gastrointestinal tract, however, RFA can be a better modality for the tumors close to the bowel. For adequate choice of modality, a multidisciplinary approach with consideration of the patient preference is essential.
Future Perspective of RTAs the irradiation technology improved, the use of SABR for liver tumors has increased. Among the advances, introduction of proton beam therapy (PBT) has led to the extended utilization of RT in liver tumors. Compared with X-ray RT, PBT has the Bragg peak phenomenon with a sharp rise and steep drop in the energy deposition along the beam path. The Bragg peak can be expanded to generate a wide range of dosimetric coverage. Due to this peculiar physical property, PBT does not lead to the exit dose that can potentially affect the normal tissue around the target volume. Because liver damage can occur even with low-dose irradiation, RILD is a main concern especially in the patients with poor liver function despite the advances in modern RT technologies. PBT, however, can reduce the irradiated volume in the normal liver parenchyma. Many studies showing the benefit of PBT in liver-directed RT were conducted in treating the HCC patients. Compared with X-ray therapy, PBT enables an increase in the prescribed dose while reducing the risk of RILD [73]. Based on this benefit of PBT, high-dose irradiation has been attempted in PBT for the HCC patients, and the 3-year LC rates of approximately ≥ 80%–85% were reported in various studies. Recently, the first phase III randomized controlled trial in which the clinical outcomes following PBT and RFA were compared among the patients with one or two recurrent HCC < 3 cm was carried out by investigators at the Korean National Cancer Center [74]. Crossover between modalities was allowed if the assigned method was not technically feasible. They reported significantly higher 2-year local progression-free survival in the PBT group on both the per-protocol population (p < 0.001) and intent-to-treat population (p < 0.001), respectively, which satisfied the non-inferiority criterion of PBT to RFA. Furthermore, the rates of crossover to the other arm were significantly higher in the RFA arm (26.4%) than in the PBT arm (8.3%), indicating that PBT was an oncologically equivalent option that could serve as an alternative for the HCC patients who were ineligible for RFA. Although the accumulating clinical evidence shows the benefit of PBT for primary HCC, relevant studies for HOCRC are still very limited. Hong et al. [75] conducted a phase II study of proton-based SABR for liver metastases from various primary tumors including CRC, pancreatic cancer, esophagogastric cancer, breast cancer, and HCC, in which the proportion of CRC patients was 38.2%. The prescribed dose was 30–50 Gy in five fractions, and the 1- and 3-year LC rates were 71.9% and 61.2%, respectively. In the CRC subgroup, the LC rates were significantly lower when compared with the total study cohort (p=0.05). Another phase II study (NCT04456621) of hypofractionated PBT for liver metastasis from various primary malignancies, with CRC of 61.2%, was performed by Kim et al. [76] and the result was published recently. The prescribed doses were mainly 60 Gy in five fractions or 70 Gy in 10 fractions. Actuarial rate of LC at 36 months was more than 60% and none of the patient developed toxicity of grade 3 or more. However, those studies dealt with liver metastasis from diverse primary cancers. There is only one currently ongoing investigation of liver-directed PBT exclusively for HOCRC (NCT03577665) [77]. The study is single-arm phase II study of curative PBT with 72 Gy in 15 fractions for patients with liver metastasis from CRC and the recruitment is ongoing. Although the data are currently limited and more results are necessary, the use of PBT in metastasis-directed therapy for HOCRC may be promising as indicated from the studies on the primary HCC patients.
Establishment of biomarkers for prognosis prediction and selection of candidates for SABR should also be investigated. mCRC has been considered radioresistant in various studies showing worse LC rate after SABR comparing with other primary malignancies [78–80]. The radioresistance of mCRC is explained by the mechanism of molecular effectors in CRC cells [81]. The expression of phosphatase of regenerating liver-3 (PRL-3) gene and survivin, the members of the inhibitor of apoptosis protein family, are specifically upregulated in mCRC comparing with other radiosensitive histologies leading the radioresistance of mCRC [81,82]. Another research by Scott et al. [83] also showed relatively low radiosensitivity of CRC by low genomic-adjusted radiation dose (GARD) of CRC among the diseases of 45 Gy level. Because GARD was derived by radiation sensitivity indices (RSIs) which were calculated based on the expression of 10 genes related with DNA-damage repair, cell cycle, or apoptosis, etc., relatively low GARD of CRC represented relatively high RSI comparing with other primary cancer cells [83]. However, the distribution of RSIs within the CRC subgroup was diverse and further analyses comparing RSIs among the CRC subgroup have not been performed [80]. Besides the differences in genetic expressions, tumor mutations including KRAS, TP53, and HER2 have attracted attention due to their possible association with curability and LC of OM patients [60]. Among the mutations, Hong et al. [75] identified the KRAS mutation as the strongest predictor of inferior LC after PBT-based SABR for liver metastasis from CRC (p=0.02). Furthermore, patients with both KRAS and TP53 mutations showed the worst 1-year LC rate compared with all other genotypes (p=0.001). For more precise selection of modality between RFA and SABR in patients with HOCRC, biomarkers for radiation sensitivity or LC rate after SABR are necessary.
Synergistic effect of RT with systemic therapy would be also an important issue. Recently, the use of immunotherapy has been extended in CRC patients especially with microsatellite instability (MSI) or mismatch repair enzymes deficiency (dMMR) as pembrolizumab showed improved progression-free survival comparing with chemotherapy in MSI-high or dMMR mCRC by KEYNOTE-177 study [84,85]. RT also induced immune modulation, in turn, sometimes resulting in the shrinkage of tumor outside the RT target, so called abscopal effect [86]. Furthermore, the immunologic effect of RT also can potentially augment the effect of immunotherapy [86]. The synergistic effect of RT and immunotherapy has been reported in various cancers [87,88]. For CRC, cases of abscopal effect after carbon-ion RT have been reported [89]. Regarding the combination of RT and immunotherapy, there were some reports support the use of RT can boost the effect of immunotherapy [90]. Especially, RT can potentially enhance the immunotherapy response in microsatellite stable CRC which is considered immunotherapy-resistant [91]. Therefore, for the patient with HOCRC who is considered as a candidate of immunotherapy, RT may potentially improve the progression-free survival by not only enhancing the response of target lesion but also suppressing elsewhere progression. However, there is no relevant study investigating the synergistic effect of immunotherapy and RT for oligometastatic CRC. Therefore, study for this issue would be meaningful.
ConclusionClassically, the life expectancy of patients with metastatic cancer was expected on a monthly basis, and only palliative systemic treatment was deemed effective. The favorable outcome of surgical resection for CRC patients with liver metastasis shows the possibility that active metastasis-directed treatment could achieve long-term survival. However, although nearly one-third of patients could have long-term survival after surgery, the rest must experience a metastatic cascade again. Therefore, the role of non-invasive approaches such as RFA and SABR, which impose a less burden on patients, has steadily increased.
RFA has been an effective tool for treating metastatic liver cancer, however, the LC rates are inferior to those for surgical resection. RFA is also not applicable to tumors located in invisible areas on ultrasonography, in an inadequate area for approach using a probe, or in an area proximal to the vasculature due to the potential heat sink effect. With advances in RT, safe liver-directed irradiation with high-dose is available, and SABR for liver tumor is widely used as complementary tool to RFA. SABR not only provides an LC similar to RFA, but also can safely treat tumors in locations that are difficult to treat with RFA, such as tumors located near major vessels, around the diaphragm, and with large size (> 2–3 cm). The introduction of particle therapy will further reduce the possible toxicities of ablative RT and maximize the efficiency by optimizing the treatment dose. The suggested decision flow is summarized in Fig. 1.
Recent clinical studies of hepatic oligometastasis from CRC investigate the combined effect with systemic treatment as well as the effectiveness of local modality. The distinctive molecular profile of oligometastasis is actively studied, that the results will enable tailored treatments for patients with metastatic disease. SABR or particle therapy is a potent non-invasive modality which can be used in conjunction with novel systemic agents to enhance the therapeutic course of CRC liver metastasis.
NotesFig. 1Suggested decision flow of local treatment for hepatic oligometastases from colorectal cancer. HOCRC, hepatic oligometastasis from colorectal cancer; RFA, radiofrequency ablation; SBRT, stereotactic body radiation therapy; US, ultrasonography. 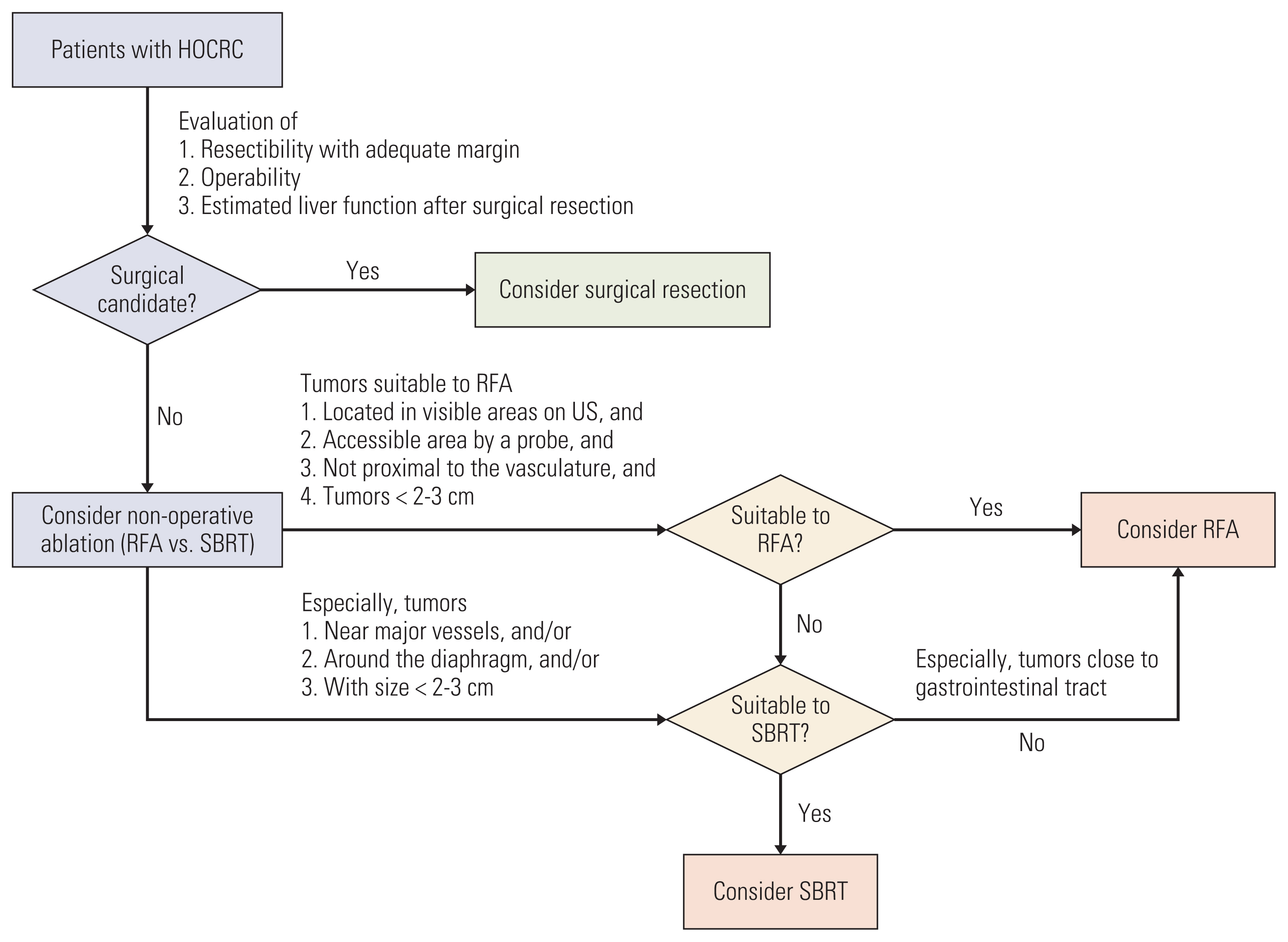
Table 1Selected studies of resection for hepatic metastasis from colorectal cancer
Table 2Selected studies comparing surgical resection and RFA for hepatic oligometastasis from colorectal cancer
Table 3Selected studies of SABR for hepatic oligometastasis from colorectal cancer
CI, confidence interval; Fx(s), fraction(s); GTV, gross tumor volume; Gr, grade; Gy10, Gy of biological effective dose with α/β=10; HR, hazard ratio; ITV, internal target volume; LC, local control; NA, not available; OS, overall survival; P, prospective study; PFS, progression-free survival; Ph, phase; SABR, stereotactic ablative body radiotherapy; R, retrospective study; TV, tumor volume. Table 4Comparison of outcomes between SABR and RFA for hepatic oligometastasis
References2. Gadd MA, Casper ES, Woodruff JM, McCormack PM, Brennan MF. Development and treatment of pulmonary metastases in adult patients with extremity soft tissue sarcoma. Ann Surg. 1993;218:705–12.
3. Hughes KS, Simon R, Songhorabodi S, Adson MA, Ilstrup DM, Fortner JG, et al. Resection of the liver for colorectal carcinoma metastases: a multi-institutional study of patterns of recurrence. Surgery. 1986;100:278–84.
4. Nordlinger B, Vaillant JC, Guiguet M, Balladur P, Paris F, Bachellier P, et al. Survival benefit of repeat liver resections for recurrent colorectal metastases: 143 cases. Association Francaise de Chirurgie. J Clin Oncol. 1994;12:1491–6.
5. Yoshino T, Arnold D, Taniguchi H, Pentheroudakis G, Yamazaki K, Xu RH, et al. Pan-Asian adapted ESMO consensus guidelines for the management of patients with metastatic colorectal cancer: a JSMO-ESMO initiative endorsed by CSCO, KACO, MOS, SSO and TOS. Ann Oncol. 2018;29:44–70.
6. Rim CH, Cho WK, Lee JH, Kim YS, Suh YG, Kim KH, et al. Role of local treatment for oligometastasis: a comparability-based meta-analysis. Cancer Res Treat. 2022;54:953–69.
7. Yoo GS, Yu JI, Park W, Huh SJ, Choi DH. Prognostic factors in breast cancer with extracranial oligometastases and the appropriate role of radiation therapy. Radiat Oncol J. 2015;33:301–9.
8. Palma DA, Olson R, Harrow S, Gaede S, Louie AV, Haasbeek C, et al. Stereotactic ablative radiotherapy for the comprehensive treatment of oligometastatic cancers: long-term results of the SABR-COMET phase II randomized trial. J Clin Oncol. 2020;38:2830–8.
9. Nevens D, Jongen A, Kindts I, Billiet C, Deseyne P, Joye I, et al. Completeness of reporting oligometastatic disease characteristics in the literature and influence on oligometastatic disease classification using the ESTRO/EORTC nomenclature. Int J Radiat Oncol Biol Phys. 2022;114:587–95.
10. Rao A, Vapiwala N, Schaeffer EM, Ryan CJ. Oligometastatic prostate cancer: a shrinking subset or an opportunity for cure? Am Soc Clin Oncol Educ Book. 2019;39:309–20.
11. Guckenberger M, Lievens Y, Bouma AB, Collette L, Dekker A, deSouza NM, et al. Characterisation and classification of oligometastatic disease: a European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus recommendation. Lancet Oncol. 2020;21:e18–28.
12. Lievens Y, Guckenberger M, Gomez D, Hoyer M, Iyengar P, Kindts I, et al. Defining oligometastatic disease from a radia-tion oncology perspective: an ESTRO-ASTRO consensus document. Radiother Oncol. 2020;148:157–66.
13. Xi Y, Xu P. Global colorectal cancer burden in 2020 and projections to 2040. Transl Oncol. 2021;14:101174.
14. National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Cancer stat facts: colorectal cancer [Internet]. Bethesda, MD: National Cancer Institute; 2022. [cited 2022 Jan 28]. Available from: https://seer.cancer.gov/statfacts/html/colorect.html
15. Biller LH, Schrag D. Diagnosis and treatment of metastatic colorectal cancer: a review. JAMA. 2021;325:669–85.
17. Riihimaki M, Hemminki A, Sundquist J, Hemminki K. Patterns of metastasis in colon and rectal cancer. Sci Rep. 2016;6:29765.
18. Rhu J, Heo JS, Choi SH, Choi DW, Kim JM, Joh JW, et al. Streamline flow of the portal vein affects the lobar distribution of colorectal liver metastases and has a clinical impact on survival. Ann Surg Treat Res. 2017;92:348–54.
19. House MG, Ito H, Gonen M, Fong Y, Allen PJ, DeMatteo RP, et al. Survival after hepatic resection for metastatic colorectal cancer: trends in outcomes for 1,600 patients during two decades at a single institution. J Am Coll Surg. 2010;210:744–55.
20. Wei AC, Greig PD, Grant D, Taylor B, Langer B, Gallinger S. Survival after hepatic resection for colorectal metastases: a 10-year experience. Ann Surg Oncol. 2006;13:668–76.
21. Leal JN, Bressan AK, Vachharajani N, Gonen M, Kingham TP, D’Angelica MI, et al. Time-to-surgery and survival outcomes in resectable colorectal liver metastases: a multi-institutional evaluation. J Am Coll Surg. 2016;222:766–79.
22. Valderrama-Trevino AI, Barrera-Mera B, Ceballos-Villalva JC, Montalvo-Jave EE. Hepatic metastasis from colorectal cancer. Euroasian J Hepatogastroenterol. 2017;7:166–75.
23. Hackl C, Neumann P, Gerken M, Loss M, Klinkhammer-Schalke M, Schlitt HJ. Treatment of colorectal liver metastases in Germany: a ten-year population-based analysis of 5772 cases of primary colorectal adenocarcinoma. BMC Cancer. 2014;14:810.
24. Van Cutsem E, Cervantes A, Adam R, Sobrero A, Van Krieken JH, Aderka D, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016;27:1386–422.
25. Scorsetti M, Comito T, Tozzi A, Navarria P, Fogliata A, Clerici E, et al. Final results of a phase II trial for stereotactic body radiation therapy for patients with inoperable liver metastases from colorectal cancer. J Cancer Res Clin Oncol. 2015;141:543–53.
26. Rusthoven KE, Kavanagh BD, Cardenes H, Stieber VW, Burri SH, Feigenberg SJ, et al. Multi-institutional phase I/II trial of stereotactic body radiation therapy for liver metastases. J Clin Oncol. 2009;27:1572–8.
27. Hughes KS, Rosenstein RB, Songhorabodi S, Adson MA, Ilstrup DM, Fortner JG, et al. Resection of the liver for colorectal carcinoma metastases: a multi-institutional study of long-term survivors. Dis Colon Rectum. 1988;31:1–4.
28. Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C, et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg. 2005;241:715–22.
29. Bogach J, Wang J, Griffiths C, Parpia S, Saskin R, Hallet J, et al. Simultaneous versus staged resection for synchronous colorectal liver metastases: a population-based cohort study. Int J Surg. 2020;74:68–75.
30. Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230:309–18.
31. Nordlinger B, Guiguet M, Vaillant JC, Balladur P, Boudjema K, Bachellier P, et al. Surgical resection of colorectal carcinoma metastases to the liver: a prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer. 1996;77:1254–62.
32. Gawdi R, Valenzuela CD, Moaven O, Stauffer JA, Del Piccolo NR, Cheung T, et al. Perioperative chemotherapy for resectable colorectal liver metastases: analysis from the Colorectal Operative Liver Metastases International Collaborative (COLOMIC). J Surg Oncol. 2022;126:339–47.
33. Tomlinson JS, Jarnagin WR, DeMatteo RP, Fong Y, Kornprat P, Gonen M, et al. Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol. 2007;25:4575–80.
34. de Jong MC, Pulitano C, Ribero D, Strub J, Mentha G, Schulick RD, et al. Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Ann Surg. 2009;250:440–8.
35. Solbiati L, Livraghi T, Goldberg SN, Ierace T, Meloni F, Dellanoce M, et al. Percutaneous radio-frequency ablation of hepatic metastases from colorectal cancer: long-term results in 117 patients. Radiology. 2001;221:159–66.
36. Curley SA, Izzo F, Delrio P, Ellis LM, Granchi J, Vallone P, et al. Radiofrequency ablation of unresectable primary and metastatic hepatic malignancies: results in 123 patients. Ann Surg. 1999;230:1–8.
37. Ruers T, Van Coevorden F, Punt CJ, Pierie JE, Borel-Rinkes I, Ledermann JA, et al. Local treatment of unresectable colorectal liver metastases: results of a randomized phase II trial. J Natl Cancer Inst. 2017;109:djx015.
38. Otto G, Duber C, Hoppe-Lotichius M, Konig J, Heise M, Pitton MB. Radiofrequency ablation as first-line treatment in patients with early colorectal liver metastases amenable to surgery. Ann Surg. 2010;251:796–803.
39. Kron P, Linecker M, Jones RP, Toogood GJ, Clavien PA, Lodge JP. Ablation or resection for colorectal liver metastases? A systematic review of the literature. Front Oncol. 2019;9:1052.
40. Gavriilidis P, Roberts KJ, de’Angelis N, Aldrighetti L, Sutcliffe RP. Recurrence and survival following microwave, radiofrequency ablation, and hepatic resection of colorectal liver metastases: a systematic review and network meta-analysis. Hepatobiliary Pancreat Dis Int. 2021;20:307–14.
41. Wang LJ, Zhang ZY, Yan XL, Yang W, Yan K, Xing BC. Radiofrequency ablation versus resection for technically resectable colorectal liver metastasis: a propensity score analysis. World J Surg Oncol. 2018;16:207.
42. Abdalla EK, Vauthey JN, Ellis LM, Ellis V, Pollock R, Broglio KR, et al. Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg. 2004;239:818–25.
43. Aloia TA, Vauthey JN, Loyer EM, Ribero D, Pawlik TM, Wei SH, et al. Solitary colorectal liver metastasis: resection determines outcome. Arch Surg. 2006;141:460–6.
44. White RR, Avital I, Sofocleous CT, Brown KT, Brody LA, Covey A, et al. Rates and patterns of recurrence for percutaneous radiofrequency ablation and open wedge resection for solitary colorectal liver metastasis. J Gastrointest Surg. 2007;11:256–63.
45. Gleisner AL, Choti MA, Assumpcao L, Nathan H, Schulick RD, Pawlik TM. Colorectal liver metastases: recurrence and survival following hepatic resection, radiofrequency ablation, and combined resection-radiofrequency ablation. Arch Surg. 2008;143:1204–12.
46. McKay A, Fradette K, Lipschitz J. Long-term outcomes following hepatic resection and radiofrequency ablation of colorectal liver metastases. HPB Surg. 2009;2009:346863.
47. Reuter NP, Woodall CE, Scoggins CR, McMasters KM, Martin RC. Radiofrequency ablation vs. resection for hepatic colorectal metastasis: therapeutically equivalent? J Gastrointest Surg. 2009;13:486–91.
48. Lee KH, Kim HO, Yoo CH, Son BH, Park YL, Cho YK, et al. Comparison of radiofrequency ablation and resection for hepatic metastasis from colorectal cancer. Korean J Gastroenterol. 2012;59:218–23.
49. Agcaoglu O, Aliyev S, Karabulut K, El-Gazzaz G, Aucejo F, Pelley R, et al. Complementary use of resection and radiofrequency ablation for the treatment of colorectal liver metastases: an analysis of 395 patients. World J Surg. 2013;37:1333–9.
50. Kim WW, Kim KH, Kim SH, Kim JS, Park SJ, Kim KH, et al. Comparison of hepatic resection and radiofrequency ablation for the treatment of colorectal liver metastasis. Indian J Surg. 2015;77:1126–30.
51. Puijk RS, Ruarus AH, Vroomen L, van Tilborg A, Scheffer HJ, Nielsen K, et al. Colorectal liver metastases: surgery versus thermal ablation (COLLISION) - a phase III single-blind prospective randomized controlled trial. BMC Cancer. 2018;18:821.
52. Comparison of hepatectomy and local ablation for resectable synchronous and metachronous colorectal liver metastasis (HELARC) [Internet]. Bethesda, MD: U.S. National Library of Medicine; 2016. [cited 2022 Jan 28]. Available from: https://clinicaltrials.gov/ct2/show/NCT02886104
53. Gurusamy K, Corrigan N, Croft J, Twiddy M, Morris S, Woodward N, et al. Liver resection surgery versus thermal ablation for colorectal LiVer MetAstases (LAVA): study protocol for a randomised controlled trial. Trials. 2018;19:105.
54. Chang DT, Swaminath A, Kozak M, Weintraub J, Koong AC, Kim J, et al. Stereotactic body radiotherapy for colorectal liver metastases: a pooled analysis. Cancer. 2011;117:4060–9.
55. Kress MS, Collins BT, Collins SP, Dritschilo A, Gagnon G, Unger K. Stereotactic body radiation therapy for liver metastases from colorectal cancer: analysis of safety, feasibility, and early outcomes. Front Oncol. 2012;2:8.
56. Burkon P, Slampa P, Kazda T, Slavik M, Prochazka T, Vrzal M. Stereotactic body radiation therapy for colorectal cancer liver metastases; early results. Klin Onkol. 2012;25 Suppl 2:2S93–7.
57. McPartlin A, Swaminath A, Wang R, Pintilie M, Brierley J, Kim J, et al. Long-term outcomes of phase 1 and 2 studies of SBRT for hepatic colorectal metastases. Int J Radiat Oncol Biol Phys. 2017;99:388–95.
58. Joo JH, Park JH, Kim JC, Yu CS, Lim SB, Park IJ, et al. Local control outcomes using stereotactic body radiation therapy for liver metastases from colorectal cancer. Int J Radiat Oncol Biol Phys. 2017;99:876–83.
59. Doi H, Uemoto K, Suzuki O, Yamada K, Masai N, Tatsumi D, et al. Effect of primary tumor location and tumor size on the response to radiotherapy for liver metastases from colorectal cancer. Oncol Lett. 2017;14:453–60.
60. Barry A, Wong R, Dawson LA. The management of colorectal cancer liver metastases: the radiation oncology viewpoint. Int J Radiat Oncol Biol Phys. 2019;103:540–1.
61. Kim YS, Lim HK, Rhim H, Lee MW, Choi D, Lee WJ, et al. Ten-year outcomes of percutaneous radiofrequency ablation as first-line therapy of early hepatocellular carcinoma: analysis of prognostic factors. J Hepatol. 2013;58:89–97.
62. Goldberg SN, Hahn PF, Tanabe KK, Mueller PR, Schima W, Athanasoulis CA, et al. Percutaneous radiofrequency tissue ablation: does perfusion-mediated tissue cooling limit coagulation necrosis? J Vasc Interv Radiol. 1998;9:101–11.
63. Kim N, Cheng J, Jung I, Liang J, Shih YL, Huang WY, et al. Stereotactic body radiation therapy vs. radiofrequency ablation in Asian patients with hepatocellular carcinoma. J Hepatol. 2020;73:121–9.
64. Kang TW, Lim HK, Lee MW, Kim YS, Choi D, Rhim H. First-line radiofrequency ablation with or without artificial ascites for hepatocellular carcinomas in a subcapsular location: local control rate and risk of peritoneal seeding at long-term follow-up. Clin Radiol. 2013;68:e641–51.
65. Rim CH, Lee HY, Kim JS, Kim H. Radiofrequency ablation and stereotactic body radiotherapy for hepatocellular carcinoma: should they clash or reconcile? Int J Radiat Biol. 2021;97:111–9.
66. Radiofrequency ablation versus stereotactic radiotherapy in colorectal liver metastases (RAS01) [Internet]. Bethesda, MD: U.S. National Library of Medicine; 2016. [cited 2022 Jan 28]. Available from: https://clinicaltrials.gov/ct2/show/NCT01233544
67. Yu J, Kim DH, Lee J, Shin YM, Kim JH, Yoon SM, et al. Radiofrequency ablation versus stereotactic body radiation therapy in the treatment of colorectal cancer liver metastases. Cancer Res Treat. 2022;54:850–9.
68. Franzese C, Comito T, Clerici E, Di Brina L, Tomatis S, Navar-ria P, et al. Liver metastases from colorectal cancer: propensity score-based comparison of stereotactic body radiation therapy vs. microwave ablation. J Cancer Res Clin Oncol. 2018;144:1777–83.
69. Stintzing S, Grothe A, Hendrich S, Hoffmann RT, Heinemann V, Rentsch M, et al. Percutaneous radiofrequency ablation (RFA) or robotic radiosurgery (RRS) for salvage treatment of colorectal liver metastases. Acta Oncol. 2013;52:971–7.
70. Vigano L, Pedicini V, Comito T, Carnaghi C, Costa G, Poretti D, et al. Aggressive and multidisciplinary local approach to iterative recurrences of colorectal liver metastases. World J Surg. 2018;42:2651–9.
71. Nieuwenhuizen S, Dijkstra M, Puijk RS, Timmer FE, Nota IM, Opperman J, et al. Thermal ablation versus stereotactic ablative body radiotherapy to treat unresectable colorectal liver metastases: a comparative analysis from the prospective Amsterdam CORE Registry. Cancers (Basel). 2021;13:4303.
72. Gotohda N, Nomura S, Doi M, Karasawa K, Ohki T, Shimizu Y, et al. Clinical impact of radiofrequency ablation and stereotactic body radiation therapy for colorectal liver metastasis as local therapies for elderly, vulnerable patients. JGH Open. 2020;4:722–8.
73. Cheng JY, Liu CM, Wang YM, Hsu HC, Huang EY, Huang TT, et al. Proton versus photon radiotherapy for primary hepatocellular carcinoma: a propensity-matched analysis. Radiat Oncol. 2020;15:159.
74. Kim TH, Koh YH, Kim BH, Kim MJ, Lee JH, Park B, et al. Proton beam radiotherapy vs. radiofrequency ablation for recurrent hepatocellular carcinoma: a randomized phase III trial. J Hepatol. 2021;74:603–12.
75. Hong TS, Wo JY, Borger DR, Yeap BY, McDonnell EI, Willers H, et al. Phase II study of proton-based stereotactic body radiation therapy for liver metastases: importance of tumor genotype. J Natl Cancer Inst. 2017;109:djx031.
76. Kim K, Yu JI, Park HC, Yoo GS, Lim DH, Noh JM, et al. A phase II trial of hypofractionated high-dose proton beam therapy for unresectable liver metastases. Radiother Oncol. 2022;176:9–16.
77. Curative proton beam therapy for patients with liver metastasis of colorectal cancer [Internet]. Bethesda, MD: U.S. National Library of Medicine; 2019. [cited 2022 Jan 28]. Available from: https://clinicaltrials.gov/ct2/show/NCT03577665
78. Lee MT, Kim JJ, Dinniwell R, Brierley J, Lockwood G, Wong R, et al. Phase I study of individualized stereotactic body radiotherapy of liver metastases. J Clin Oncol. 2009;27:1585–91.
79. Oh D, Ahn YC, Seo JM, Shin EH, Park HC, Lim DH, et al. Potentially curative stereotactic body radiation therapy (SBRT) for single or oligometastasis to the lung. Acta Oncol. 2012;51:596–602.
80. Ahmed KA, Caudell JJ, El-Haddad G, Berglund AE, Welsh EA, Yue B, et al. Radiosensitivity differences between liver metastases based on primary histology suggest implications for clinical outcomes after stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys. 2016;95:1399–404.
81. Anuja K, Chowdhury AR, Saha A, Roy S, Rath AK, Kar M, et al. Radiation-induced DNA damage response and resistance in colorectal cancer stem-like cells. Int J Radiat Biol. 2019;95:667–79.
82. Bardelli A, Saha S, Sager JA, Romans KE, Xin B, Markowitz SD, et al. PRL-3 expression in metastatic cancers. Clin Cancer Res. 2003;9:5607–15.
83. Scott JG, Berglund A, Schell MJ, Mihaylov I, Fulp WJ, Yue B, et al. A genome-based model for adjusting radiotherapy dose (GARD): a retrospective, cohort-based study. Lancet Oncol. 2017;18:202–11.
84. Andre T, Shiu KK, Kim TW, Jensen BV, Jensen LH, Punt C, et al. Pembrolizumab in microsatellite-instability-high advanced colorectal cancer. N Engl J Med. 2020;383:2207–18.
85. Diaz LA Jr, Shiu KK, Kim TW, Jensen BV, Jensen LH, Punt C, et al. Pembrolizumab versus chemotherapy for microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer (KEYNOTE-177): final analysis of a randomised, open-label, phase 3 study. Lancet Oncol. 2022;23:659–70.
86. Pevzner AM, Tsyganov MM, Ibragimova MK, Litvyakov NV. Abscopal effect in the radio and immunotherapy. Radiat Oncol J. 2021;39:247–53.
87. Torok JA, Salama JK. Combining immunotherapy and radiotherapy for the STAR treatment. Nat Rev Clin Oncol. 2019;16:666–7.
88. Ngwa W, Irabor OC, Schoenfeld JD, Hesser J, Demaria S, Formenti SC. Using immunotherapy to boost the abscopal effect. Nat Rev Cancer. 2018;18:313–22.
89. Ebner DK, Kamada T, Yamada S. Abscopal effect in recurrent colorectal cancer treated with carbon-ion radiation therapy: 2 case reports. Adv Radiat Oncol. 2017;2:333–8.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||