AbstractPurposeTropomyosin receptor kinase (TRK) inhibitors are approved for the treatment of neurotrophic receptor tyrosine kinase (NTRK) fusion-positive tumors. The detection of NTRK fusion using a validated method is required before therapeutic application. An interlaboratory comparison study of next-generation sequencing (NGS)–based NTRK gene fusion detection with validated clinical samples was conducted at six major hospitals in South Korea.
Materials and MethodsA total of 18 samples, including a positive standard reference and eight positive and nine negative clinical samples, were validated using the VENTANA pan-TRK (EPR17341) and TruSight Oncology 500 assays. These samples were then tested using four different NGS panels currently being used at the six participating institutions.
Results
NTRK fusions were not detected in any of the nine negative clinical samples, demonstrating 100% specificity in all six participating institutions. All assays showed 100% analytical sensitivity to identify the NTRK fusion status in formalin-fixed paraffin-embedded (FFPE) samples, although with variable clinical sensitivity. False-negative results were due to low tumor purity, poor RNA quality, and DNA-based sequencing panel. The RNA-based targeted NGS assay showed an overall high success rate of identifying NTRK fusion status in FFPE samples.
ConclusionThis study is the first to test the proficiency of NGS-based NTRK detection in South Korea with the largest participating institutions. RNA-based NGS assays to detect NTRK fusions can accurately characterize fusion transcripts if sufficient RNA of adequate quality is available. The comparative performance data will support the implementation of targeted NGS-based sequencing assays for NTRK fusion detection in routine diagnostics.
IntroductionThe neurotrophic receptor tyrosine kinase (NTRK) family of genes includes three, NTRK1, NTRK2, and NTRK3, that encode tropomyosin receptor kinases (TRK) A, B, and C, respectively [1]. A rearrangement involving one of the genes in this family represents a significant oncogenic event in various cancers [2,3]. Fusions involving a kinase domain of the NTRK gene lead to uncontrolled activation and overexpression of tyrosine receptor kinase [1].
Several different TRK inhibitors are currently investigated for clinical application (larotrectinib, entrectinib, selitrectinib, and repotrectinib). Of these agents, Larotrectinib is a highly selective TRK inhibitors [4] and has received accelerated approval by the US Food and Drug Administration in November 2018 and has subsequently been approved in more than 40 other countries [5]. First published clinical results of 55 larotrectinib-treated pediatric and adult patients with NTRK fusion-positive advanced solid tumors showed an overall response rate of 76% and progression-free survival of 79% after 12 months of treatment [6]. An integrated analysis of larotrectinib in the three trials (phase 1 for adults, phase 2 for adults and adolescents, and phase 1–2 for pediatric), was higher (75% vs. 57%) than in the integrated analysis of entrectinib reported responses, although direct comparisons between individual trials are difficult due to considerable differences in the population of enrolled patients achieving an objective and study design [7].
To qualify for the former treatment, tumors must have an NTRK fusion gene without known acquired resistance mutations. However, the NTRK fusions are a wide variety of gene fusion partners and possible breakpoints at different exons of the NTRK tyrosine kinase domain [8,9]. Therefore, it is important to investigate the diagnostics that are best suited to identify a wide range of different NTRK fusion variants in formalin-fixed paraffin-embedded (FFPE) tissue with variable tumor cell contents in routine practice. The US Food and Drug Administration recently approved the next-generation sequencing (NGS)–based FoundationOne CDx test (Foundation Medicine Inc., San Diego, CA) as a companion diagnostic tool to identify fusions including NTRK genes in DNA isolated from tumor tissue specimens from patients with solid tumors eligible for treatment with larotrectinib in October 2020 [10]. However, a suggested limitation of the FoundationOne CDx is that a subset of patients with solid tumors with NTRK1/2/3 fusions may be missed.
This study aimed to compare the ability of four different targeted RNA and DNA sequencing assays to reliably detect NTRK gene fusions in FFPE samples via joint research conducted by six major hospitals in Korea. Here, we present the sensitivity, specificity, and limitations of the assays used in routine practice by each institution to identify fusions in NTRK.
Materials and Methods1. Sample collectionFFPE tumor tissue blocks were cut into 5 μm thick sections and stained with hematoxylin and eosin. To detect the expression of TRK, all samples were stained using the VENTANA pan-TRK (EPR17341) assay kit (Roche Diagnostics, Indianapolis, IN) according to the manufacturer’s instructions. Although there is no scoring algorithm or criteria to determine immunohistochemistry (IHC) positivity, positive staining has been defined as at least 1% of tumor cells in any pattern including cytoplasmic, membranous, perinuclear and nuclear staining, as described in recent studies [11,12]. The presence of NTRK fusion gene was confirmed using a targeted RNA panel assay (SOLIDaccuTest RNA, NGeneBio, Seoul, Korea). Based on IHC and NGS analysis, eight NTRK fusion gene-positive and nine negative samples were selected; the positive samples included the NTRK1 (n=4), NTRK2 (n=1), and NTRK3 (n=3) fusion genes. Samples that had sufficient residual tumor tissue and had been prepared recently based on when the tissue was resected were selected preferentially.
2. Case preparationFor the NGS assays, institution A—the organizing institution—prepared a total of 18 samples, including eight positive clinical samples with the NTRK gene fusion and nine negative clinical samples screened using the VENTANA pan-TRK (EPR17341) assay kit and a positive control sample from SeraCare (0710-1031, Seraseq FFPE NTRK Fusion RNA Reference, Milford, MA). Seventeen clinical samples, excluding standard substances, were validated using the TruSight Oncology (TSO) 500 assay (Illumina Inc., San Diego, CA). The eight positive samples were confirmed by an additional hybridization capture-based targeted RNA panel (SOLIDaccuTest RNA) that included all NTRK1/2/3 exons. Seventeen FFPE tissue samples were cut with a 5 μm curl for analysis at each institution (Fig. 1) and assigned numbers based on the cutting order (Table 1). Seraseq FFPE NTRK fusion RNA was also prepared as a standard substance. The RNA reference was a 10 μm curl and had 15 clinically relevant NTRK gene fusions in a single reference sample (S1 Table). The curls were then stored in an e-tube (study ID BN01-BN18), and two e-tubes per sample were delivered to the participating institutions in a dry ice box. The DNA/RNA was prepared for further analysis according to the protocol at each institution. The samples were then tested using the NGS panel currently used at each institution according to the protocol used in actual clinical practice. Given that the study design used a paraffin sample, the cutting order of the sample could affect the percentage of tumor cells, namely the purity of the tumor, in the sample. Therefore, to avoid bias in the sample selection, the marked curl numbers (1 [top]–12 [bottom]) in each tube were assigned randomly (Table 1) and distributed evenly to each institution.
3. NGS assays to detect NTRK fusionThree different RNA panels and one DNA panel used to diagnose patients at each hospital were tested to detect the fusion of the NTRK gene. Institutions A and E used TSO 500, institution B used Lung Cancer Panel v3.0, and institutions C and F used Oncomine Comprehensive Assay v3 (OCA v3), and institution D used OncoPanel v.4.3. The OncoPanel v.4.3 and Lung Cancer Panel v3.0 were developed in-house in each institution; OncoPanel v.4.3 is DNA-based.
4. TSO 500DNA (40 ng) was quantified using the Qubit dsDNA HS Assay (Thermo Fisher Scientific, Waltham, MA) on a Qubit 2.0 Fluorometer (Thermo Fisher Scientific), then sheared using a Covaris E220 Focused-ultrasonicator (Woburn, MA) and the 8 microTUBE–50 Strip AFA Fiber V2 following manufacturer’s instructions. The treatment time was optimized for FFPE material. The treatment settings were as follows: peak incident power (W), 75; duty factor, 15%; cycles per burst, 500; treatment time (seconds), 360; temperature (°C), 7; water level, 6. The DNA library was prepared and enriched using the TSO 500 Kit (Illumina); manufacturer’s instructions were followed. Post-enriched libraries were quantified, pooled, and sequenced using NextSeq 500 (Illumina). The quality of the NextSeq 500 sequencing runs was assessed using Illumina Sequencing Analysis Viewer (Illumina). Sequencing data were analyzed using the TSO 500 Local App ver. 1.3.0.39 (Illumina). The TSO 500 is a comprehensive tumor profiling assay designed to identify known and emerging tumor biomarkers, including small variants, splice variants, and fusions. Importantly, the TSO 500 measures tumor mutational burden (TMB) and microsatellite instability, which are potentially key biomarkers for immunotherapy. TMB was reported as mutations per megabase (Mb) sequenced, and a high TMB was defined as mutations of more than 10 per Mb (≥ 10 Mut/Mb).
5. OncoPanel v.4.3Genomic DNA was isolated from each section of FFPE tissue using a NEXprep FFPE Tissue kit (NexK-9000, Genes Laboratories, Seongnam, Korea), according to the manufacturer’s protocol. Tissue pellets were lysed completely by overnight incubation with proteinase K in lysis buffer at 56°C, followed by additional incubation for 3 minutes with magnetic beads and solution A at 37°C. After incubation for 5 minutes on a magnetic stand, the supernatants were removed and washed 3 times with ethanol. After the beads were air-dried for 5 minutes, DNA was eluted in 50 μL of nuclease-free water and quantified using a Qubit dsDNA HS Assay kit (Thermo Fisher Scientific). Targeted NGS was performed using the NextSeq platform (Illumina) with OncoPanel v.4.3, designed in-house by the Center for Cancer Genome Discovery at institution D to target a total of 328 genes (808 kb), including a complete exonic sequence of 225 genes, 105 hot spots, and a partial intronic sequence of six genes. A DNA library was prepared by fragmenting gDNA (200 ng) to an average of 250 bp using S1 enzyme, followed by sequential reactions of end repair, A tailing, and ligation of 50 ng of purified DNA using a TruSeq adaptor, using a SureSelectXT Reagent kit (Agilent Technologies, Santa Clara, CA). Each library was addressed with sample-specific barcodes of 6 bp and quantified using Qubit. Eight libraries were pooled to a total of 750 ng for hybrid capture using an Agilent SureSelectXT custom kit (OncoPanel ver. 4.3 RNA bait, Agilent Technologies). The concentration of the enriched target was measured using a quantitative polymerase chain reaction (Kapa Biosystems, Woburn, MA) and the sample was loaded onto the NextSeq platform (Illumina) for paired-end sequencing.
6. Lung Cancer Panel v3.0Lung Cancer Panel v3.0 is a laboratory-developed DNA- and RNA-based NGS assay to target 75 DNA genes (DNA) and 21 genes (RNA), respectively, including MET exon 14 skipping events along with prominent fusions. For the DNA-based assay, a library was prepared using the SureSelect XT-HS Target Enrichment System (Agilent Technologies) and the RNA-based assay utilized the anchored multiplex polymerase chain reaction method (ArcherDx, Boulder, CO) to enrich targets. Paired-end sequencing was performed on the Illumina NextSeq 550Dx platform (Illumina).
7. Oncomine Comprehensive Assay v3For library preparation, the multiplex PCR-based Ion Torrent AmpliSeq technology (Life Technologies, Thermo Fisher Scientific) with the Oncomine Comprehensive Assay v3 (IonTorrent, Thermo Fisher Scientific) was used. The OCA v3 allows concurrent analysis of DNA and RNA to detect multiple types of variants across 161 solid tumor–related genes simultaneously in a single workflow. Amplicon library preparation was performed using the Ion AmpliSeq Library Kit v2.0 (Thermo Fisher Scientific). Briefly, 20 ng of genomic DNA was mixed with the two primer pools and the AmpliSeq HiFi Master Mix before they were transferred to a PCR cycler (Bio-Rad, Munich, Germany). For detection of gene–fusions, RNA was reverse transcribed using the SuperScript VILO cDNA Synthesis Kit according to the manufacturer’s instructions (Thermo Fisher Scientific). The amplicon libraries were prepared from 20 ng RNA, which were mixed with two primer pools and the AmpliSeq HiFi Master Mix before transferring them to a PCR cycler (Bio-Rad). Subsequently, DNA respectively RNA pools were combined and primer end sequences were partially digested using FuPa reagent, followed by the ligation of barcoded sequencing adapters using the Ion Xpress Barcode Adapters 1–48 Kit (Thermo Fisher Scientific). The purified libraries were quantified using the Ion Library TaqMan Quantitation Kit (Thermo Fisher Scientific).
Results1. NGS analysis of NTRKAll five participating institutions, apart from the organizing institution (institution A), were blinded to the NTRK fusion status of the samples analyzed. All six participating institutions performed analyses using NGS-based targeted DNA and RNA sequencing assays implemented in their laboratories. All six institutions submitted their results within the given deadline and successfully completed the NGS analysis of NTRK.
2. Clinicopathological characteristics in 17 clinical samples and 1 NTRK fusion RNA as a standard substanceThe samples used in the test were surgical tissues from solid cancer patients diagnosed from 2013–2020 without oncogenic driver alterations (ALK, ROS1, BRAF, and EGFR in lung cancer; EGFR, KRAS, NRAS, and BRAF in colon cancer). The NTRK fusion-positive samples were first selected through VENTANA pan-TRK IHC staining (Fig. 2) and further validated with the TSO 500 assay and an additional hybridization capture-based targeted RNA panel assay (SOLIDaccuTest RNA). Detailed information on the samples used in the tests is summarized in Table 2. Clinical samples were derived from 13 male and four female patients, and the median age at diagnosis was 53 years (range, 23 to 72 years). The eight NTRK fusion-positive samples were detected in six different types of solid cancer, including colorectal adenocarcinoma (n=3), inflammatory myofibroblastic tumor of the lung (n=1), secretory carcinoma of the salivary gland (former World Health Oragnization classification: mammary analogue secretory carcinoma; n=1), glioblastoma of the brain (n=1), prostate stromal sarcoma (n=1), and mucinous adenocarcinoma of uncertain origin (n=1). The median tumor purity of the sample was 60%, with a range of 20%–90%. The eight NTRK fusion-positive samples consisted of four cases of NTRK1 fusion (TPR-NTRK1 [1], TPM3-NTRK1 [3]), one case of NTRK2 fusion (HOOK3-NTRK2), and three cases of NTRK3 fusion (ETV6-NTRK3 [2], RBPMS-NTRK3 [1]) (Table 3). Of the eight NTRK fusions, ETV6-NTRK3 and TPM3-NTRK1 were highly prevalent NTRK fusion variants whereas the remainder were low-frequency NTRK fusions.
Reference standards for monitoring the analytical performance of the assay were incorporated in the analysis. The Seraseq FFPE NTRK fusion RNA is a reference standard containing a total of 15 clinically relevant NTRK fusion genes in a single reference sample (TPM3-NTRK1, LMNA-NTRK1, IRF-2BP2-NTRK1, SQSTM1-NTRK1, TFG-NTRK1, AFAP1-NTR-K2, NACC2-NTRK2, QKI-NTKR2, TRIM24-NTRK2, PAN3-NTRK2, ETV6-NTKR3, and BTBD1-NTRK3). Further detailed information on this is provided in S1 Table.
3. Sensitivity and specificity of NTRK fusion detection by NGS analysis in 17 clinical samplesNo fusion reads were observed in any of the nine NTRK fusion-negative samples, demonstrating 100% specificity at all six participating institutions. The sensitivity of the NTRK fusion detection differed between the institutions. The detected fusion supporting read counts and curl order delivered to each institution are described in Table 4. The Lung Cancer Panel v3.0 (institution B) and TSO 500 (institution E) assays showed 100% analytical and clinical sensitivity at detecting the eight NTRK-positive samples. The TSO 500 (institution A), OCA v3 (institutions C and F), and OncoPanel v.4.3 (institution D) assays showed 87.5% (A), 87.5% (C), 75% (F), and 37.5% (D) clinical sensitivity, respectively, but 100% analytical sensitivity.
The ETV6-NTRK3 fusion-positive sample (BN01) with highly prevalent NTRK fusion variants was not detected in the TSO 500 (institution A), OCA v3 (institution F), and OncoPanel v.4.3 (institution D) assays. This sample (BN01) initially had the lowest tumor purity (20%). The samples with latter curl numbers (11 and 12) did not present any tumor cells in the sample, resulting in a failure to detect ETV6-NTRK3 fusion.
Unfortunately, two cases (BN04 and BN07) failed RNA quality control in the OCA v3 assay (institution C). The cutting order of these two samples was curl numbers 1 and 2. Curl numbers 1 and 2 are the uppermost sections of FFPE tissue.
The OCA v3 panel did not include the HOOK3-NTRK2 fusion gene; therefore, it was not detected at the two institutions that used it. Although other fusion isoforms of TPR-NTRK1 were included in the OCA v3 assay, the TPR-NTRK1 (T4N10) fusion case in the ring study was not a target. Hence, in the OCA v3 assay (institution F), a TPR-NTRK1 (T4N10) fusion (BN03) was detected but filtered out because it was not annotated according to the criteria used by the Oncomine Variant Annotator. Later, the TPR-NTRK1 (T4N10) fusion was found with high fusion read counts (94,492) in manual inspections.
The OncoPanel v.4.3 assay (institution D) was the only DNA-based sequencing panel included in this study. NTRK fusion was not detected in any of the four cases (BN01, 04, 10, and 13).
4. Detection of Seraseq, the NTRK fusion referenceThe NTRK fusion supporting read counts detected are shown in Table 5. Only the TSO 500 assay covered 100% of the 15 NTRK fusion genes presented in the Seraseq NTRK fusion transcripts. The TSO 500 assay (institutions C and F) successfully detected all 15 NTRK fusion genes. However, the OCA v3 assay did not include PAN3-NTRK2 among the 15 NTRK fusion genes. The results from the two institutions using the OCA v3 assay showed seven discordant cases. The OCA v3 assay used at institution C failed to detect LMNA-NTRK1 and PAN3-NTRK2 while that used at institution F initially failed to detect IRF2BP2-NTRK1, SQSTM1-NTRK1, TFG-NTRK1, AFAP1-NTRK2, TRIM24-NTRK2, PAN3-NTRK2, ETV6-NTR-K3 (E4N15), and ETV6-NTRK3 (E4N14) according to annotation criteria used with Oncomine Variant Annotator. We analyzed the seven discordant cases further by performing a manual review of variant calling. The TFG-NTRK1 fusion variant was a non-targeted fusion, i.e., not targeted with the original primer combination; it was later found, with high read counts (read counts: 114,933), via manual inspection. In addition, the SQSTM1-NTRK1, AFAP1-NTRK2, TRIM24-NTRK2, ETV6-NTRK3 (E4N15), and ETV6-NTRK3 (E4N14) variants were detectable with low amounts of transcript reads (range, 3 to 33) in the OCA v3 assay at F institution. At least 40 reads of a specific fusion were required to call it a fusion variant. Therefore, the SQSTM1-NTRK1, AFAP1-NTRK2, TRIM24-NTRK2, ETV6-NTRK3 (E4N15), and ETV6-NTRK3 (E4N14) variants were initially filtered out because they were not annotated given the low number of transcript reads. The IRF2BP2-NTRK1 fusion variant was not identified by the OCA v3 assay at institution F and showed a low amount of transcript reads (read count, 112) with the same assay at institution C. Eventually, only one case of a discrepancy was identified between the two institutions using the OCA v3 assay. Unfortunately, the LMNA-NTRK1 fusion variant was not identified in two institutions using the OCA v3 assay despite the assay including that fusion variant. The amplicon-based OCA v3 assay detected 100% of all highly prevalent fusions (ETV6-NTRK3 and TPM3-NTRK1) but was able to detect just 80% of the less frequent fusion variants. The Lung Cancer Panel v3.0 assay (institution B) detected 13 NTRK fusion genes presented in Seraseq NTRK fusion transcripts, but the NACC2-NTRK2 and TRIM24-NTRK2 fusion variants were not identified. The results from the Lung Cancer Panel v3.0 assay were similar to those from the OCA v3 assay; it detected 100% of all highly prevalent fusions but only 80% of the less frequent ones.
Lastly, OncoPanel v.4.3 (institution D) could not be tested using the NTRK fusion reference RNA sample because it was a DNA-based NGS assay.
DiscussionThis was a multi-centric comparative study for NGS-based detection of NTRK fusion. The six institutions participating in this study have the highest number of patients and conduct the largest number of NGS tests in Korea. The NGS instruments are operated with the approval of the Ministry of Food and Drug Safety and quality control by the Korea Institute of Genetic Testing and Evaluation. This study is the first proficiency test involving the participation of the most institutions with NGS-based NTRK detection facilities in Korea. Conducting such studies is challenging because of the scarcity of NTRK-positive clinical samples and because it was not feasible to test sufficient numbers at each institution. Thus, although there is an obvious need for such a ring study, one had not been conducted previously as a matter of routine.
Analytical sensitivity indicates how well a test can detect specific molecules, namely it can only evaluate technical performance, whereas clinical sensitivity is affected by pre-analytical factors other than technical performance. We analyzed separately clinical and analytical sensitivity, since this ring study have pre-analytical factors that may not occur when applied in under real diagnostics. RNA-based targeted NGS assays showed 100% analytical sensitivity and specificity, regardless of test panels and superior clinical sensitivity than DNA-based targeted NGS assays.
NTRK fusions can be detected using multiple technologies, such as IHC, reverse transcription polymerase chain reaction, fluorescence in situ hybridization, and NGS [13]. The pan-TRK IHC has the advantage of being easy to use, cheap, and immediately applicable; however, based on the results to date, there is a limit to its use as a method of patient selection given its 44%–100% sensitivity and 46%–100% specificity [14]. NGS performance had a high specificity (99%) and moderately high sensitivity (> 90%) for each variant, except for single nucleotide variants (99%), in each clinical laboratory. Therefore, the guidelines for the detection of NTRK fusions recommend either confirmation by NGS after screening by IHC or immediate implementation of NGS. There are two representative methods of target enrichment in NGS: the amplification method used in the Thermo Fisher OCA v3 assay and the hybridization capture method used in the TSO 500 assay.
The majority of NTRK fusions occur at very low frequencies in a variety of common cancers—such as lung adenocarcinoma, colorectal and papillary thyroid carcinomas, and sarcoma—with the exception of several rare specific tumor types that are highly enriched for NTRK fusion (secretory breast carcinoma and secretory carcinoma of salivary gland, infantile fibrosarcoma, and congenital mesoblastic nephroma) [15–19].
Furthermore, NTRK gene fusions—unlike ALK gene fusions—exhibit a wide variety of gene fusion partners [8,9]. Therefore, as many of these partners are not fully covered by amplicon-based assays such as the OCA v3 used in this study, other reports on NTRK fusion detection have noted hybridization capture as providing more advantages. A hybrid capture-based assay, such as the TSO 500 used in the current study, was designed to identify gene fusions that are currently unknown; this is advantageous for the broad spectrum of NTRK fusion partners. However, the advantage of the OCA v3 assay is that only 20 ng of RNA was needed to prepare the library; this is lower than the amounts required in other assays (40–200 ng). Therefore, OCA v3 can be an effective confirmatory tool, following IHC screening, for detecting already targetable gene fusions in cases where only small biopsies are possible.
Sample types included both DNA and RNA; similar to previous reports, the highest detection rate was obtained with NGS using RNA [12,20,21]. Recent reports have also shown that DNA-based sequencing panels can lead to false-negative fusion results [20,22] owing to the design and inherent limitations of the sequencing technology applied. Most breakpoints on the DNA level are located in intronic/intergenic regions that may not be fully covered because of the size of the gene [23]. Additionally, when such breakpoints can occur in repetitive GC-rich sequences their detectability in these genetic regions is strongly impaired [23]. Therefore, DNA-based NGS can lead to false negatives of NTRK fusions, particularly those involving NTRK2 and NTRK3 as these have large intronic regions. Therefore, additional RNA sequencing assays are recommended.
All DNA- and RNA-based NGS assays used in this ring study are currently being used in routine diagnostics. Even if all tests were conducted according to their respective protocols, the detection rates might have varied depending on factors known to affect NGS assay results, such as sample preparation, processing method, and data analysis. NGS testing utilizing RNA, in particular, can be more complicated and demanding than other single-gene tests; therefore, they would require a careful procedure by the institution conducting the test.
The sensitivity of the targeted NGS assay can be limited by pre- and post-analytical factors. Pre-analytical tissue selection plays a key role in the success of NGS analysis. To ensure the selection of appropriate tissue, most institutions must select appropriate surgical tissue sections that best meet the requirements of the RNA-based NGS assay. It is necessary to optimize RNA inputs based on tumor cellularity or withhold poor quality samples from library preparation, because it is inevitable that FFPE samples would be used for RNA sequencing in a routine clinical setting. Thus NGS analysis of NTRK fusion may lack sensitivity, particularly in cases of low tumor cellularity. In such samples, negative fusion results do not fully imply a lack of fusion. In this ring study, the ETV6-NTRK3 fusion-positive clinical sample (BN01) had the lowest tumor purity (20%) although it is a highly prevalent NTRK fusion variant. The samples with latter curl numbers (11 and 12) did not present any tumor cells in the sample, resulting in a failure to detect ETV6-NTRK3 fusion. Half of the institutions participating in this ring study did not detect the ETV6-NTRK3 fusion. Therefore, although the typical minimum tumor content requirement for NGS analysis is theoretically 10%–20%, more than 30% is required in real diagnostics.
Exposure of FFPE sections to light and air may negatively influence RNA quality. This is another concern that is different from that related to low tumor purity in the pre-analytic phase. However, storing entire FFPE blocks either in the open or protected from air and light will ensure that RNA quality is not affected as long as the uppermost section is discarded. Unfortunately, two cases (BN04 and BN07) failed RNA quality control in the OCA v3 assay (institution C). The cutting order of these two samples was curl numbers 1 and 2, which were the uppermost sections of FFPE tissue; therefore, the exposure of the FFPE tissue section to air, resulting in “oxidation,” has been assumed to be related to the failure [24]. To prevent “oxidation,” sections not directly exposed to air should be used for RNA preparation [24]. The false-negative result from the TSO 500 assay (institution A) could be presumed to be due to oxidation (curl numbers 1 and 2) or low tumor purity. In this ring study, the uppermost sections that were directly exposed to air were not discarded and these might have influenced RNA quality. In this ring trial, FFPE tissue samples were cut with a 5 μm curl for analysis at each participating institution, with the curls then stored in an e-tube before delivery there. Therefore, this pre-analytical factor is a limitation of this ring study that may not be applicable to real diagnostics.
The next issue is related to post-analytical factors such as sophisticated bioinformatics. In the OCA v3 assay used at institution F, several variants with non-targeted fusion and a low abundance of transcripts were absent in the initial output from the software Ion Reporter. Adjusting the analysis parameters and conducting a re-analysis resulted in the identification of the variants, indicating that these variants had been successfully sequenced but filtered out by the bioinformatics pipeline. In OCA v3, non-targeted fusions with either novel fusion partners or novel breakpoints were also reported by assessing the significance of supporting mapped sequencing read information [25]. Non-targeted fusion variants were detected but filtered out because they were not annotated according to the annotation criteria with the Oncomine Variant Annotator. However, the analysis of new combinations of existing primer pairs can lead to the identification of fusions beyond those for which the assay was originally designed. Therefore, a non-targeted fusion variant that was not present in the original target list could be detected in an OCA v3 assay. Our analysis identified two fusions (TPR-NTRK1 and TFG-NTRK1) for which the calling algorithm identified “non-targeted” fusion transcripts obtained from primer combinations that were not initially designed as pairs in the OCA v3 assay used at institutions C and F.
Furthermore, at least 40 reads of a specific fusion were required—in the OCA v3 assay—to call the fusion a variant. Initially, several variants with fewer than 40 read counts were filtered out because they were not annotated because of the low number of transcript reads. The minimum number of fusion supporting reads for positive calling differed for each assay. Therefore, to detect rare but clinically significant RNA fusions, the count of unique supporting reads for the fusion–given the detection limit based on tumor purity–should be considered as making a positive fusion call via an adjustment of analysis parameters.
In conclusion, the RNA-based targeted NGS assay showed an overall high success rate of identification of NTRK fusion status in FFPE samples. The ability of an RNA-based targeted NGS assay to detect NTRK fusions depended on pre- and post-analytical factors as well as the technology used in routine practice. RNA-based targeted NGS assays to detect NTRK fusions can accurately characterize fusion transcripts if sufficient RNA of adequate quality is available. Therefore, an RNA-based targeted NGS assay to detect NTRK fusion can be established in a routine diagnostic setting, if applied considering the limitations identified in this ring trial. The comparative performance data will support the implementation of an RNA-based targeted NGS assay for NTRK fusion detection in routine diagnostics and will be helpful in setting up or proceeding with NTRK NGS tests elsewhere.
Electronic Supplementary MaterialSupplementary materials are available at Cancer Research and Treatment website (https://www.e-crt.org).
NotesEthical Statement A total of six institutes participated in the ring trial and analyses were conducted on four different NGS panels. This retrospective cohort study was approved by the Institutional Review Board of each institution (institution A: 2020-05-095; institution B: H-2009-056-1155; Institution C: KC20SIDI0651; institution D: 2020-1386; institution E: 4-2020-0721; institution F: KUMC 2020-09-031) and performed in accordance with the principles of the Declaration of Helsinki. The requirement for informed consent was waived. Author Contributions Conceived and designed the analysis: Lee SE, Lee MS, Choi YL. Collected the data: Lee SE, Lee MS, Choi YL. Contributed data or analysis tools: Lee SE, Lee MS, Jeon YK, Shim HS, Kang J, Kim J, Choi YL. Performed the analysis: Lee SE, Lee MS, Jeon YK, Shim HS, Kang J, Kim J, Choi YL. Wrote the paper: Lee SE, Lee MS, Kim J, Choi YL. AcknowledgmentsThis study was supported by National Research Foundation of Korea (NRF) grants funded by the Korean government (Ministry of Science, ICT and Future Planning) (NRF-2016R1A5A2945889 and 2019R1A2B5B0269979).
Fig. 1Overview cutting of the tumor tissue slices with formalin-fixed paraffin-embedded (FFPE) blocks. Seventeen FFPE tissue samples were cut with a 5 μm curl for next-generation sequencing analysis and curls were numbered according to the order of cut followed by placed in a microcentrifuge tube. Two vials were assigned to each institution. IHC, immunohistochemistry; TRK, tropomyosin receptor kinase. 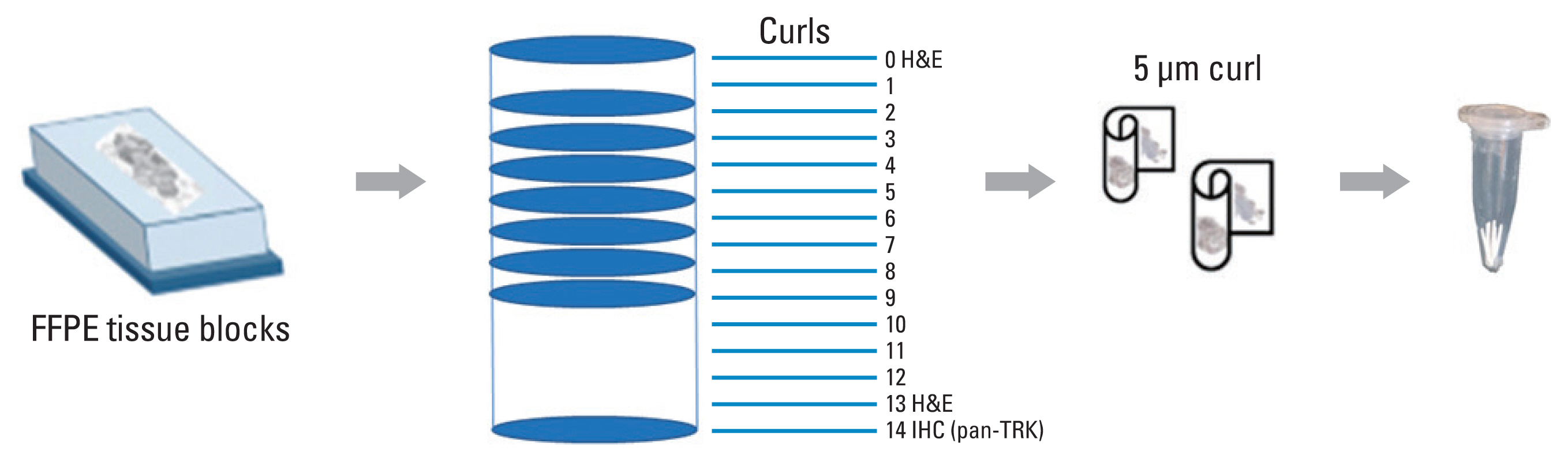
Fig. 2Tumor histology and pan–tyrosine receptor kinase (TRK) staining of ring trial samples. Resected formalin-fixed paraffin-embedded (FFPE) samples were stained with VENTANA pan-TRK (EPR17341) assay kits; cases determined to be positive for staining were further validated for neurotrophic receptor tyrosine kinase (NTRK) fusion gene detection via additional next-generation sequencing (NGS) analysis. Samples BN01, BN03, BN04, BN07, BN10, BN11, BN13, and BN17 were confirmed as positive by NGS analysis; these are marked in red. BN16 is a reference obtained from Seraseq FFPE NTRK Fusion RNA and is not an experimental sample. 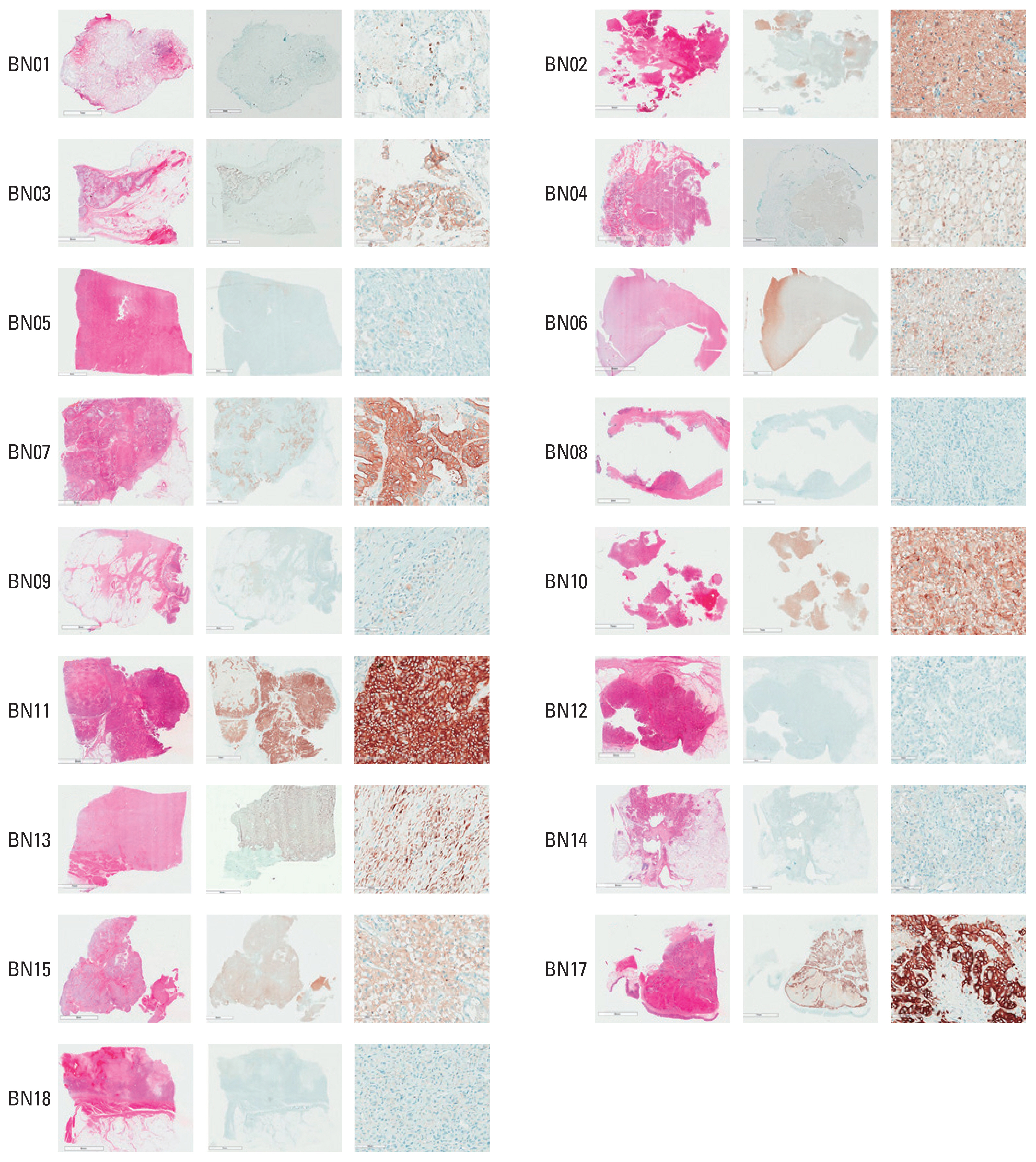
Table 1Tissue cuts assigned at each institution Table 2Clinicopathological characteristics in 17 clinical samples Table 3
NTRK fusion-positive samples list confirmed with the TSO 500 assay
Table 4Analytical sensitivity of NGS assays for NTRK fusion-positive samples by institution
Table 5
NTRK fusion transcripts detected from Seraseq, NTRK fusion reference
References1. Vaishnavi A, Le AT, Doebele RC. TRKing down an old oncogene in a new era of targeted therapy. Cancer Discov. 2015;5:25–34.
2. Cocco E, Scaltriti M, Drilon A. NTRK fusion-positive cancers and TRK inhibitor therapy. Nat Rev Clin Oncol. 2018;15:731–47.
3. Okamura R, Boichard A, Kato S, Sicklick JK, Bazhenova L, Kurzrock R. Analysis of NTRK alterations in pan-cancer adult and pediatric malignancies: implications for NTRK-targeted therapeutics. JCO Precis Oncol. 2018;2018:PO.1800183.
4. Federman N, McDermott R. Larotrectinib, a highly selective tropomyosin receptor kinase (TRK) inhibitor for the treatment of TRK fusion cancer. Expert Rev Clin Pharmacol. 2019;12:931–9.
6. Chen Y, Chi P. Basket trial of TRK inhibitors demonstrates efficacy in TRK fusion-positive cancers. J Hematol Oncol. 2018;11:78.
7. Doebele RC, Drilon A, Paz-Ares L, Siena S, Shaw AT, Farago AF, et al. Entrectinib in patients with advanced or metastatic NTRK fusion-positive solid tumours: integrated analysis of three phase 1–2 trials. Lancet Oncol. 2020;21:271–82.
8. Gatalica Z, Xiu J, Swensen J, Vranic S. Molecular characterization of cancers with NTRK gene fusions. Mod Pathol. 2019;32:147–53.
9. Hsiao SJ, Zehir A, Sireci AN, Aisner DL. Detection of tumor NTRK gene fusions to identify patients who may benefit from tyrosine kinase (TRK) inhibitor therapy. J Mol Diagn. 2019;21:553–71.
10. FDA approves companion diagnostic to identify NTRK fusions in solid tumors for Vitrakvi [Internet]. Silver Spring MD: U.S. Food and Drug Administration; 2020. [cited 2021 Dec 10]. Available from: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-companion-diagnostic-identify-ntrk-fusions-solid-tumors-vitrakvi
11. Hechtman JF, Benayed R, Hyman DM, Drilon A, Zehir A, Frosina D, et al. Pan-Trk immunohistochemistry is an efficient and reliable screen for the detection of NTRK fusions. Am J Surg Pathol. 2017;41:1547–51.
12. Solomon JP, Linkov I, Rosado A, Mullaney K, Rosen EY, Frosina D, et al. NTRK fusion detection across multiple assays and 33,997 cases: diagnostic implications and pitfalls. Mod Pathol. 2020;33:38–46.
13. Penault-Llorca F, Rudzinski ER, Sepulveda AR. Testing algorithm for identification of patients with TRK fusion cancer. J Clin Pathol. 2019;72:460–7.
14. Xu B, Haroon Al Rasheed MR, Antonescu CR, Alex D, Frosina D, Ghossein R, et al. Pan-Trk immunohistochemistry is a sensitive and specific ancillary tool for diagnosing secretory carcinoma of the salivary gland and detecting ETV6-NTRK3 fusion. Histopathology. 2020;76:375–82.
15. Bourgeois JM, Knezevich SR, Mathers JA, Sorensen PH. Molecular detection of the ETV6-NTRK3 gene fusion differentiates congenital fibrosarcoma from other childhood spindle cell tumors. Am J Surg Pathol. 2000;24:937–46.
16. Davis JL, Lockwood CM, Albert CM, Tsuchiya K, Hawkins DS, Rudzinski ER. Infantile NTRK-associated mesenchymal tumors. Pediatr Dev Pathol. 2018;21:68–78.
17. Rubin BP, Chen CJ, Morgan TW, Xiao S, Grier HE, Kozakewich HP, et al. Congenital mesoblastic nephroma t(12;15) is associated with ETV6-NTRK3 gene fusion: cytogenetic and molecular relationship to congenital (infantile) fibrosarcoma. Am J Pathol. 1998;153:1451–8.
18. Skalova A, Vanecek T, Sima R, Laco J, Weinreb I, Perez-Ordonez B, et al. Mammary analogue secretory carcinoma of salivary glands, containing the ETV6-NTRK3 fusion gene: a hitherto undescribed salivary gland tumor entity. Am J Surg Pathol. 2010;34:599–608.
19. Tognon C, Knezevich SR, Huntsman D, Roskelley CD, Melnyk N, Mathers JA, et al. Expression of the ETV6-NTRK3 gene fusion as a primary event in human secretory breast carcinoma. Cancer Cell. 2002;2:367–76.
20. Benayed R, Offin M, Mullaney K, Sukhadia P, Rios K, Desmeules P, et al. High yield of RNA sequencing for targetable kinase fusions in lung adenocarcinomas with no mitogenic driver alteration detected by DNA sequencing and low tumor mutation burden. Clin Cancer Res. 2019;25:4712–22.
21. Solomon JP, Hechtman JF. Detection of NTRK fusions: merits and limitations of current diagnostic platforms. Cancer Res. 2019;79:3163–8.
22. Haynes BC, Blidner RA, Cardwell RD, Zeigler R, Gokul S, Thibert JR, et al. An integrated next-generation sequencing system for analyzing DNA mutations, gene fusions, and RNA expression in lung cancer. Transl Oncol. 2019;12:836–45.
23. Pfarr N, Kirchner M, Lehmann U, Leichsenring J, Merkelbach-Bruse S, Glade J, et al. Testing NTRK testing: Wet-lab and in silico comparison of RNA-based targeted sequencing assays. Genes Chromosomes Cancer. 2020;59:178–88.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||