INTRODUCTION
An esophageal carcinoma is often diagnosed at an advanced stage and only a small number of patients can be considered for curative resection and thus, for long-term survival (1). Surgical resection remains the only curative treatment modality for an esophageal carcinoma without distant metastasis (2). Therefore, it is important to detect distant metastases in patients with an esophageal carcinoma, so that unwarranted surgery can be avoided. Despite the increase in radical surgery for esophageal carcinomas, about 43~63% of patients eventually experience a recurrent disease after surgery (3,4). Thirty to forty percent of recurrences are due to hematogenous spread, and common sites of recurrence are the liver, lung, bone and adrenal glands. The kidney is known to be the 4th or 5th most common visceral metastasis site of esophageal carcinomas (5~7). However, solitary renal metastasis of an esophageal squamous cell carcinoma has rarely been reported. Herein, a case of solitary, unilateral renal metastasis in a patient with curatively resected, thoracic esophageal carcinoma, who achieved a complete remission after preoperative concurrent chemoradiotherapy, is reported.
CASE REPORT
A 64-year-old man was admitted with an evaluation of progressive dysphagia in November, 2001. He had complained of dysphagia for the previous 2 months. An endoscopy showed a circular ulcerofungating mass measuring 4 cm in length, 32 cm from the incisor. A biopsy revealed a moderately differentiated, invasive squamous cell carcinoma. Staging work-up, including endoscopic ultrasonography, chest CT, abdominal CT and PET scan, showed a right high paratracheal lymph node enlargement, without distant metastasis. Under the diagnosis of locally advanced esophageal cancer, he received pre-operative concurrent chemoradiation therapy, consisting of 2 cycles of cisplatin (75 mg/m2) on day 1 and 5-fluorouracil (1,000 mg/m2) on days 1 to 4, which was repeated every 3 weeks. Radiation therapy was delivered in a total dose of 4,500 cGy in 25 fractions. He underwent an Ivor-Lewis operation, with 2-field lymph node dissection, on January 21, 2002. A histological examination showed no residual malignant cells or metastatic foci in 17 regional dissected lymph nodes, suggesting a pathologically complete remission after the preoperative chemoradiotherapy.
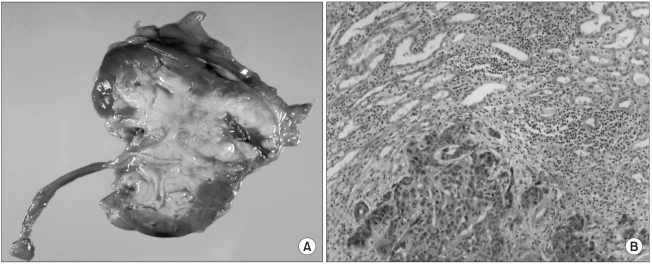
During the regular post-operative follow-up as an outpatient, a solitary left kidney mass was detected in December, 2003. The patient was asymptomatic, with no abdominal discomfort, hematuria or any other urinary symptoms. A kidney CT scan revealed a heterogeneously attenuating mass lesion approximately 4.1×3.4 cm in size, with persistent weak enhancement on the anterior lip, mid-portion of the left kidney (Fig. 1). There were no other visceral metastases or lymphadenopathies in the CT scan. A PET scan (Fig. 1) also showed a single, abnormal increased uptake of the left kidney. He underwent a radical nephrectomy on January 14, 2004. A histological examination of the resected kidney showed a metastatic squamous cell carcinoma, which coincided with the histological findings of the previously resected esophageal carcinoma (Fig. 2). The follow-up abdominal CT scan revealed suspicious metastatic lymphadenopathy in the para-aortic space. The patient received palliative chemotherapy, consisting of cisplatin 75 mg/m2 on day 1 and continuous infusion of 1,000 mg/m2 5-fluorouracil on days 1 to 4. After 3 cycles of chemotherapy, the size of the suspicious paraaortic lymphadenopathy had decreased in extent in the follow-up CT scan.
DISCUSSION
The incidence of distant metastases from a newly diagnosed esophageal carcinoma has been reported as approximately 18% (6). Several autopsy series reported that the common sites of spread as being abdominal lymph nodes (45%), followed by the liver (35%), lung (20%), cervical & supraclavicular lymph nodes (18%), bone (9%), adrenal glands (5%), peritoneum (2%) and brain (2%). Of these, the frequencies of visceral metastatic spread were as follows: lung, 22~52%; liver, 23~47%; adrenal glands, 6~20%; bone, 4~14%; kidney, 8~13% and central nervous system, 1~5% (5,8,9).
Because the renal blood flow accounts for approximately 20% of cardiac output, the kidneys are likely to be vulnerable to hematogenous metastases. More than 50% of renal metastases typically show bilateral involvement. The clinical manifestation of a metastatic renal tumor differs from that of primary renal cell carcinoma in several aspects. The majority of primary renal cell carcinomas are, on average, larger than metastatic renal tumor, with most primary tumors measuring over 6 cm at the time of presentation, compared with less than 4 cm for metastatic tumors. Second, metastases tend to be less exophytic and wedge-shaped than a primary renal cell carcinoma (10~12). Metastatic renal tumors are frequently observed in subcapsular location, which can be explained by a tumor seeding into the vascular renal cortex, with subsequent elongated growth being limited by the renal capsule, which produces a wedge shaped appearance.
The majority of patients with renal metastases are asymptomatic, despite extensive renal involvement. Hematuria and/or proteinuria occur in less than 20% of patients, and a cytologic examination infrequently shows malignant cells in the urine. Therefore, the diagnosis of renal metastases is very difficult, and often established accidentally (12~14). Renal metastasis from a primary esophageal carcinoma is commonly found in autopsy series, but is rarely diagnosed in live patients. Moreover, unilateral, solitary renal metastasis is extremely rare. Yokoi et al reported that G-CSF and CA19-9 may play a role in attaching the metastatic tumor cells to the glomerular endothelium (14). Further investigations are necessary to identify the molecules and cytokines involved in renal metastasis.
In this case, the patient achieved a pathologic complete remission after preoperative concurrent chemotherapy with irradiation. About 2 years after the curative resection, the patient recurred with a solitary renal metastasis. Since current diagnostic tools can not detect all the micrometastatic sites of a disease, the usefulness of curative nephrectomy cannot be determined in this clinical setting. A nephrectomy could be justified in limited situations, such as with the uncertainty of histological diagnosis, severe life-threatening hematuria which cannot be controlled by embolization, or solitary renal metastasis with a long disease free interval.
The median survival following the detection of a recurrent esophageal carcinoma is 5.0~7.0 months (1,2). The treatment outcome of a recurrent disease is disappointing, and the prognosis is notoriously poor. Therefore, molecular biological techniques for determining the tumor biology are needed to identify patients who will experience a recurrence. More early detection methods and effective systemic therapeutic modalities of esophageal carcinomas are also required.