Pembrolizumab for Refractory Metastatic Myxofibrosarcoma: A Case Report
Article information
Abstract
Myxofibrosarcoma is a rare tumor, refractory to cytotoxic chemotherapy and radiotherapy. Pembrolizumab is an innovative immunotherapy drug consisting of programmed death receptor ligand 1 antibody proven to be useful for numerous types of cancer cells. A patient had been diagnosed with metastatic myxofibrosarcoma, refractory to radiotherapy and conventional cytotoxic chemotherapy. The patient achieved a partial response during palliative chemotherapy with pembrolizumab for 14 cycles. To the best of our knowledge, this is the first case report demonstrating the efficacy of pembrolizumab for refractory myxofibrosarcoma.
Introduction
Myxofibrosarcoma (MFS) is a subset of soft tissue sarcoma, which occasionally presented as a heart problem because of its myxoid portion [1]. In previous studies, wide excision and adjuvant radiotherapy was considered as standard treatment for operable MFS, and palliative chemotherapy could be used in selective patients with metastatic MFS; however, it is difficult to treat due to a high rate of recurrence and distant metastases [2]. Pembrolizumab, an innovative immunotherapy drug, is the first programmed death receptor ligand 1 (PD-L1) inhibitor approved by U.S. Food and Drug Administration (FDA) and has shown promising results in solid tumors [3-7].
In this report, we present the case of a 45-year-old man with refractory metastatic MFS, who received pembrolizumab and achieved partial response for 18 months. The Institutional Review Board of Gyeongsang Hospital approved this retrospective case study and waived the requirement for informed consent.
Case Report
A 45-year-old man was diagnosed with MFS with a left axillary mass and underwent surgical resection and received adjuvant radiation therapy, 5,400 cGy, on the resection site on September 2015. After radiotherapy, he was re-hospitalized for dyspnea because of multiple lung metastases and received one cycle of palliative chemotherapy composed of etoposide, ifosfamide, and cisplatin on November 2015. However, his disease progressed.
He was admitted with cardiac arrest on March 2016. The initial electrocardiogram revealed ST segment elevation (Fig. 1A), and coronary angiography showed total occlusion of the mid-left anterior descending artery caused by thrombus formation (Fig. 1B). Aspiration thrombectomy was successfully performed. The aspirated specimens were sent to the Department of Histopathology, and he was diagnosed with metastatic high-grade sarcoma (Fig. 2). Immunohistochemical examination confirmed a diagnosis of primary MFS. The patient was transferred to the oncology department for treatment.

(A) Electrocardiogram showing ST segment elevation in leads V2 to V5. (B) Coronary angiography image showing complete occlusion at the mid-left anterior descending artery (arrow).

Histopathologic findings of aspirated specimens: anaplasia and pleomorphism of the nucleus compatible with high-grade metastatic sarcoma (H&E staining, ×40).
A computed tomography (CT) scan showed pulmonary vein and left atrium invasion from multiple lung metastases and that a coronary embolism from a lobulated mass in the left atrium caused the cardiac arrest (Fig. 3A).
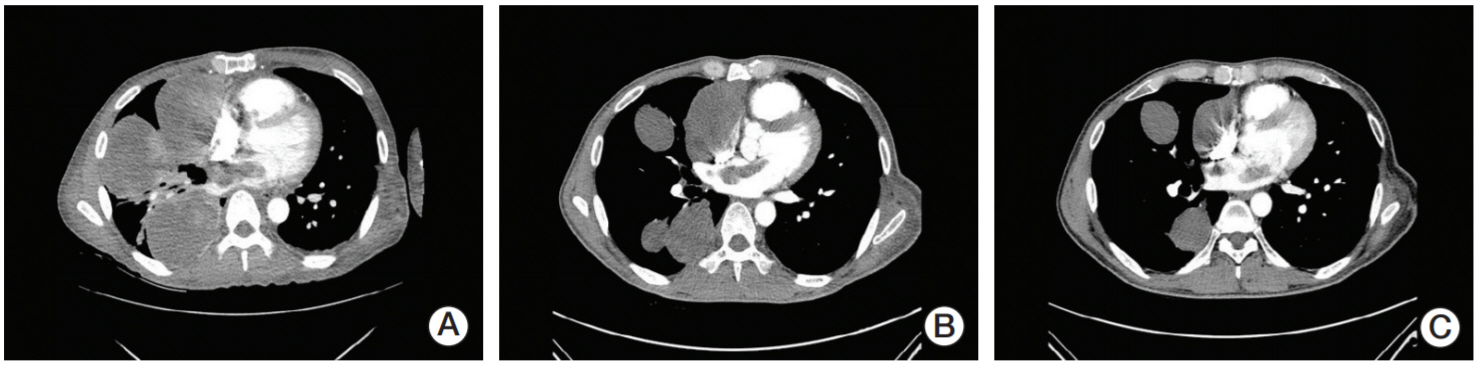
(A) Baseline chest computed tomography (CT) image shows multiple metastatic lung mass with tumor invasion to the left atrium from the pulmonary vein. (B) Follow-up CT image shows a partial response after two cycles of pembrolizumab and a slight decrease in the size of the multiple masses in both the lung and left atrium. (C) Follow-up CT image shows a partial response after four cycles of pembrolizumab and a marked decrease in the size of the multiple masses in both the lung and left atrium.
Although the disease was in an advanced stage, the patient and his family desired palliative chemotherapy. Given the poor cardiac function, adriamycin-containing regimen was not suitable for chemotherapy. Thereafter, he received 2 mg/kg of pembrolizumab via intravenous infusion every 3 weeks. A partial response was achieved after two cycles of pembrolizumab (Fig. 3B). Moreover, his performance status improved, and the symptoms, including dyspnea and pain, completely subsided. CT images after four cycles showed a decrease in the size of the masses in both the lung and left atrium (Fig. 3C). He received ten additional cycles of pembrolizumab in an outpatient setting without any side effects. Unfortunately, the patient died from incidental intracranial hemorrhage after 18 months since receiving pembrolizumab.
Discussion
MFS is a subtype of soft tissue sarcoma, composed of malignant fibroblasts with a myxoid matrix. Currently, the World Health Organization recognizes MFS as a disease distinct from myxoid malignant fibrous histiocytoma [8]. The standard of treatment for MFS is a wide excision [2]. However, MFS shows high rates of local relapse after surgery; therefore, adjuvant radiotherapy should be performed. Unfavorable outcomes of MFS are associated with a large tumor size, deep location, high histologic grade, and positive resection margin [3].
Despite the efforts to control local recurrence, 15%-38% of locally relapsed MFS develop distant metastases [9]. Palliative chemotherapy could be used in patients with metastatic MFS; however, effective and standardized chemotherapeutic regimens do not exist because of its rarity.
We present the case of a patient with conventional chemotherapy-refractory metastatic MFS who received pembrolizumab as palliative immunotherapy. MFS lacks genetic and molecular evidence for using targeted chemotherapeutic agents. Pembrolizumab is a highly selective, humanized monoclonal IgG4-kappa isotype antibody against PD-L1. Anti‒PD-L1 antibodies can reverse negative immune regulatory signaling pathways of cytotoxic T cells. Pembrolizumab has shown robust clinical activity with an acceptable safety profile for various types of solid tumors [4].
In previous studies, biomarkers to predict clinical benefit from pembrolizumab were established. For example, preexisting CD8+ T cells in the tumor microenvironment were required for tumor regression after pembrolizumab [10]. Moreover, higher numbers of PD-1+ T cells at baseline and increased PD-L1 expression during treatment were associated with clinical response of receiving pembrolizumab [11]. The role of PD-L1 expression in soft tissue sarcoma was previously investigated. In one analysis, expression of PD-L1 was significantly associated with a poor outcome, especially in soft tissue sarcoma rather than bone sarcoma [12]. Another study demonstrated that PD-L1 expression was present in 15% of all sarcomas (34/222). By histologic types, undifferentiated pleomorphic sarcomas had the highest prevalence of PD-L1 expression; otherwise, MFS showed a negative PD-L1 expression [13].
Tawbi et al. [14] described that pembrolizumab showed clinically meaningful responses in patients with undifferentiated pleomorphic sarcoma or dedifferentiated liposarcoma, rather than bone sarcoma. Although no patients with MFS were enrolled in this study, one patient with chemotherapyrefractory MFS receiving nivolumab achieved complete response in another study [15].
To the best of our knowledge, this report represents the first evidence of pembrolizumab exhibiting efficacy against refractory metastatic MFS without any toxicity. In conclusion, we believe pembrolizumab could be an option for controlling metastatic sarcoma, including MFS without degrading the patient’s quality of life. Further studies of the efficacy and biomarkers of pembrolizumab for refractory metastatic sarcoma are warranted.