INTRODUCTION
MATERIALS AND METHODS
1) Subjects
2) Isolation of cancer cells, elimination of normal cells, and tissue culture
3) Anticancer drug treatment and ATP assay
AbstractPurposeA chemosensitivity test can reflect the differences in responses of individual cancer patients to chemotherapeutic agents. The adenosine triphosphate-based chemotherapy response assay (ATP-CRA)is an accurate method, which does not require a large amount of tissue specimen. So far, no studies have evaluated the utility of the ATP-CRA in Korea. Therefore, we investigated the clinical usefulness of the ATP-CRA in 53 patients with lung cancer.
Materials and MethodsTumor tissues were obtained from bronchoscopic biopsies or surgical resections. The validity of ATP-CRA was assessed focusing on the success rate, experimental error level (intraassay mean coefficient of variation [CV]) and reproducibility.
ResultsThe overall success rate of ATP-CRA was 90.6% (48/53). Normal cells were effectively eliminated from the tumor tissues with the use of ficoll gradient centrifugation and immunomagnetic separation, which was confirmed using loss of heterozygosity analysis of the 3p deletion. The mean CV of ATP assays was 10.5±4.6%. The reproducibility of ATP assays was 94±3.8%. The results of the ATP assays were reported to physicians within 7 days of specimen collection. More than 6 anticancer drugs were tested on the tumor specimens obtained from bronchoscopic biopsies.
INTRODUCTIONLung cancer is the leading cause of cancer death in Korea (1). Anticancer chemotherapy is the main treatment modality for small cell lung cancer (SCLC) and advanced non-small cell lung cancer (NSCLC). In some recent studies, a survival benefit has been demonstrated with adjuvant chemotherapy in patients with completely resected NSCLC (2,3). Thus, the importance of anticancer chemotherapy for lung cancer is being reappraised.
The chemosensitivity test (CST) is an in vitro predictive assay for assessing the sensitivity of cancer cells to various chemotherapeutic agents, but poses some problems that limit its application in clinical practice; for example, it is time-consuming (14 to 21 days), has a low success rate (less than 60%) and requires a large amount of tissue specimens (4). The ATP-based chemosensitivity test (ATP assay) has some advantages over other CSTs; it is more sensitive in predicting cell viability, eliminates or suppresses normal cells from tumor tissues and does not require a large amount of specimens (5~8). Intracellular ATP is the basic energy source for all living cells, and disappears rapidly when cells lose their viabilities. Loss of cell viability after treatment with chemotherapeutic agents results in decreased cellular ATP levels. Thus, an ATP assay can analyze the cytotoxic effects of anticancer drugs by measuring the amount of ATP. Its clinical applications to melanomas, and ovarian, breast and stomach cancers have been reported (9~17). Recently, correlations between drug sensitivity in the ATP assay and the survival benefit in patients with ovarian cancer were observed (16,17).
So far, no studies have evaluated the utility of the ATP assay in Korea. Therefore, we conducted this study to investigate clinical usefulness of the ATP assay in patients with lung cancer, focusing on the success rate, experimental error level and reproducibility.
MATERIALS AND METHODS1) SubjectsFifty-three patients, who underwent a bronchoscopic biopsy (n=45), or surgical resection (n=8) for the diagnosis and treatment of lung cancer at The Severance Hospital, Yonsei University College of Medicine, between December 2003 and February 2005, were included in this study. An informed consent for participation was obtained from all patients.
2) Isolation of cancer cells, elimination of normal cells, and tissue cultureTumor tissues stored in HBSS (GIBCO BRL Rockville, MD), containing 100 IU/ml penicillin (Sigma, St Louis, MO), 100 µg/ml streptomycin (Sigma), 100 µg/ml gentamicin (GIBCO BRL), 2.5 µg/ml amphotericin B (GIBCO BRL) and 5% fetal bovine serum (FBS, GIBCO BRL), were delivered to the laboratory. These tissues underwent washing, quantification and mincing, followed by incubation with extracellular matrix-degrading enzymes, such as dispase (Sigma), pronase (Sigma) and DNase (Sigma), at 37℃ for 12 to 16 hours. Cells were harvested using a cell strainer (BD Falcon, Bedford, MA). To eliminate normal cells, the cell suspensions were subjected to ficoll (1.077 g/ml) gradient centrifugation, at 400 g for 15 min, and anti-CD45 antibody conjugated magnetic beads (Miltenyi Biotech, Auburn, CA). The viability of isolated cells was tested using trypan blue exclusion. A QIAamp DNA mini Kit (QIAGEN, Hilden, Germany) was used for DNA extraction from cancer and normal tissues, and from cells collected after enzymatic disaggregation, ficoll gradient centrifugation and immunomagnetic separation. In the cases of surgically resected tissues, normal tissues adjacent to tumors were also obtained for the purpose of a 3p deletion analysis. PCR was performed using three loss of heterozygosity (LOH) markers (D3S1611, D3S1612 and D3S1300) specific to the short arm of chromosome 3; with LOH analysis performed using a Genetic Analyzer (Applied Biosystems, Foster City, CA). The histological types of the tumor tissues, as well as qualitative and quantitative analyses of cancer cells were evaluated by two pathologists (H Kim and D-H Shin).
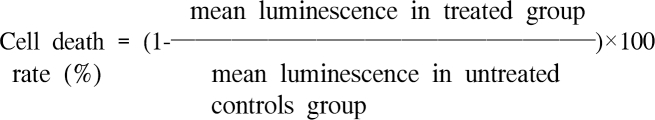
3) Anticancer drug treatment and ATP assaySeparated tumor cells were diluted to 2,000~20,000 viable cells/100 µl using IMDM (GIBCO BRL), including 10% FBS, and seeded in triplicate to a 96-well ultra low attachment microplate (Costar, Cambridge, MA), which was able to restrict growing normal cells, such as fibroblasts. In the treated groups, 100 µl of chemotherapeutic agents were added on the seeded cells and cultured for 48hrs in a CO2 incubator. In the untreated control groups, 100 µl of IMDM, without chemotherapeutic agents, was added to 3~6 wells of the microplate. For the purpose of quality control, a negative control group of 3~6 wells (only seeding medium without cells) and two positive control groups were included in the culture plate. Each positive control group was composed of 3 wells that contained the minimal (105 pg ATP) and median (280 pg ATP) amounts of ATP, as measured in 1,000 tumor cells harvested from tissue. The final concentrations of anticancer drugs were determined by training set experiments, which exhibited scattered distribution of cell deaths from each specimen (data not shown); cisplatin (2.5 µg/ml), carboplatin (12 µg/ml), paclitaxel (8.5 µg/ml), docetaxel (3.7 µg/ml), gemcitabine (16.9 µg/ml), vinorelbine (0.18 µg/ml) and irinotecan (4.7µg/ml). Cells from the untreated control and treated groups were lysed, and the amounts of ATP in the cell lysates measured using luciferin and excessive luciferase (Roche, Mannheim, Germany), followed by flash type luminescence measurements on a Victor 3 multi-label counter (PerkinElmer Boston, MA). The cell death rate for each drug was calculated as follows:
 To calculate the intraassay mean coefficient of variation (CV) value, luminescence values of each specimen were measured 3 times. We then confirmed whether the measured values at 280 pg of ATP were higher than those at 105. If there were microorganism contamination, inadequate number of cells and an intraassay mean CV greater than 30, the test was considered a failure. If the measured values in the untreated control were lower than those in the positive group (105 pg of ATP), the specimen was considered to have unacceptable viability. The subject of assay reproducibility testing was confined to the tissues obtained from surgical resections, and the ATP-CRA performed by different examiners. A comparative method was used to compare the area displayed in the cell death graph (18).
RESULTS1) Success rate of tissue culture and isolation of cancer cellsOf the 53 patients, 5 were excluded from this study due to the following reasons: three tumor specimens had unacceptable viabilities for obtaining reliable results, as the measured values of the untreated control were lower than those of the positive control group (105 pg ATP), microorganism contamination was observed in one specimen, and one specimen did not yield an adequate number of cells. All 5 of these tumor specimens were obtained from bronchoscopic biopsies. The success rates of ATP-CRA using specimens from surgical resections or bronchoscopic biopsies were 100 (8/8) and 88.9% (40/45), respectively, with an overall success rate of ATP-CRA was 90.6% (48/53). The number of specimens per patient obtained from bronchoscopic biopsies varied from 2 to 6 pieces. The mean weight of the tissues obtained from the bronchoscopic biopsies and surgical resections were 25.4±15.1 mg (mean±standard deviation [SD]) and 329.4±202.6 mg, respectively. The mean viability of cells separated by enzymatic disaggregation was 93.3±7.1%. The mean number of cells acquired per 1mg of cancer tissue was 28,323±31,111. Lung cancer cells were present in all 48 specimens. The histological types of lung cancer were as follows; small cell lung cancer (n=5), adenocarcinoma (n=23), squamous cell carcinoma (n=17), adenosquamous carcinoma (n=2) and pleomorphic carcinoma (n=1) (Table 1).
2) Evaluation of normal cell elimination
Table 2 and Fig. 1 show representative results of the two patients. A normal cell eliminating effect was observed at D3S1300 in patient 1, which became clear after the ficoll gradient centrifugation. In patient 2, normal cell eliminating effects were observed at D3S1611 and D3S1612, but these became obvious only after additional immunomagnetic separation. PCR-LOH analysis was not feasible for tissues with homozygosity. One patient (patient 1) exhibited no allelic loss at the D3S1611 marker.
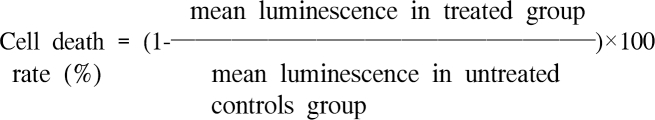
3) Chemosensitivity of lung cancer cells measured by ATP assayThe results of the ATP-CRA were reported within 7 days of obtaining the tumor tissue in all cases. The number of chemotherapeutic agents tested per tumor specimen for all cases and from the bronchoscopic biopsies were 6.3±1.4 (mean±SD; range, three to 12) and 6.2±1.3, respectively. Using the tissues obtained from surgical resections, all chemotherapeutic agents available were tested for the ATP-CRA. The list of chemotherapeutic agents tested, and their corresponding results, are presented in Table 3. The cytotoxic effects for the same concentration of the chemotherapeutic agents on cell death ranged from 0 to 77% (Table 3, Fig. 2). Cisplatin showed the highest median cell death rate value (39.8%) and the widest range of cytotoxic effects (6.5~76.7%). Irinotecan showed the lowest median cell death rate value (4.5%) and gemcitabine showed the narrowest range of cytotoxic effects (0~48%). The measured values of the negative control group were low enough to be ignored, and no reverse tendency of measured values between the two positive control groups was observed. The mean CV of the ATP-CRA was 10.5±4.6% (range, 3.3 to 21.8). In 2 of the surgically resected specimens, two examiners performed reproducibility tests using equally-divided specimens. In 4 other surgically resected specimens, three examiners performed reproducibility tests by dividing the specimens into 3 pieces, and the results compared. A total of 14 reproducibility tests were performed. The mean value of reproducibility was 94±3.8% (range, 86.7 to 99.2%).
DISCUSSIONChemosensitivity tests can reflect differences in the response of individual cancer patients to chemotherapeutic agents. The in vitro chemosensitivity assays showed an overall sensitivity and specificity of 85 and 80%, respectively (19). Recently, a meta-analysis demonstrated that the response rate to assayguided chemotherapy was slightly higher than that with standard chemotherapy (27 vs. 18%) when CST was applied in clinical practice (20).
The ATP assay can be performed with a very small amount of cancer tissue, and effectively eliminates or suppresses normal cells from the tissue specimens and is more accurate than previous CSTs, such as the MTT assay (5~8). Therefore, the ATP assay is widely used in Western countries. In this study, the ATP assay was applied to patients with lung cancer to investigate its clinical utility as a CST.
The results of the ATP-CRA were reported to physicians within 7 days of specimen collection; thus, chemotherapy could be initiated without any delay. The success rate of the ATP-CRA was 90.6%, which was similar or even superior to those in other countries (10,13~15,17,21). The mean CV of the test was 10.5%, which was also superior to a previous study (13.0%) (21). High reproducibility rates were observed for all cases when the tests were repeated by different examiners. The ATP-CRA could be applied to specimens obtained from bronchoscopic biopsies using more than 6 anticancer drugs. From the above results, the ATP-CRA was confirmed to be a stable, accurate and potentially practical CST method in patients with lung cancer.
All CST involve a process that directly measures the number of viable cells after treatment with cytotoxic drugs. Early methods measured the ability of living cells to form colonies or to uptake isotope-labeled thymidine, while recent methods measure the number of living cells from the amount of ATP, dehydrogenase enzyme activity (MTT, HDRA) and integrity of cell membrane (DiSC) in order to shorten the turnaround time and improve the success rates (22). Contrary to the DiSC assay, which is dependent on the morphologic differences between cancer and normal cells, the measurement of the amount of ATP or the enzyme activity may be affected by contaminated normal cells within the cancer tissue (23,24). Therefore, it is important to eliminate and inhibit the proliferation of normal cells. In this study, we demonstrated that normal cells were effectively eliminated from the tumor tissue using ficoll gradient centrifugation and CD45 immunomagnetic separation.
A wide range of cell deaths was observed in this study. Cisplatin, which forms the backbone of lung cancer chemotherapy, showed the greatest cytotoxic effect in vitro. Our previous study on the validation of APT-CRA for NSCLC patients predicted the response rates with a sensitivity and specificity of 83.3 and 100%, respectively (25). Although the feasibility of the CST has been established for more than 25 years, a clear clinical benefit of assay-guided chemotherapy remains to be adequately demonstrated in lung cancer. To define the clinical benefit of assay-guided chemotherapy based on the above results, a clinical trial targeting patients with stages IIIB or IV has been initiated at our institute. We are currently comparing the response rates and ultimately survival outcomes of in vitro best regimens, which are composed of cisplatin and other chemotherapeutic agent showing the most cytotoxic effects in the ATP-CRA, to empiric chemotherapy.
References1. National Statistics OfficeAnnual Report of Death Statistics Data in 2003. Korea:
2. The International Adjuvant Lung Cancer Trial Collaborative GroupCisplatin-based adjuvant chemotherapy in patients with completely resected non-small-cell lung cancer. N Engl J Med. 2004;350:351–360. PMID: 14736927
3. Kato H, Ichinose Y, Ohta M, Hata E, Tsubota N, Tada H, et al. A randomized trial of adjuvant chemotherapy with uracil-tegafur for adenocarcinoma of the lung. N Engl J Med. 2004;350:1713–1721. PMID: 15102997
4. Salmon SE, Hamburger AW, Soehnlen B, Durie BG, Alberts DS, Moon TE. Quantitation of differential sensitivity of human-tumor stem cells to anticancer drugs. N Engl J Med. 1978;298:1321–1327. PMID: 77475
5. Maehara Y, Anai H, Tamada R, Sugimachi K. The ATP assay is more sensitive than the succinate dehydrogenase inhibition test for predicting cell viability. Eur J Cancer Clin Oncol. 1987;23:273–276. PMID: 3109921
6. Petty RD, Sutherland LA, Hunter EM, Cree IA. Comparison of MTT and ATP-based assays for the measurement of viable cell number. J Biolumin Chemilumin. 1995;10:29–34. PMID: 7762413
7. Cree IA, Kurbacher CM. Individualizing chemotherapy for solid tumors-is there any alternative? Anticancer Drugs. 1997;8:541–548. PMID: 9300568
8. Andreotti PE, Cree IA, Kurbacher CM, Hartmann DM, Linder D, Harel G, et al. Chemosensitivity testing of human tumors using a microplate adenosine triphosphate luminescence assay: clinical correlation for cisplatin resistance of ovarian carcinoma. Cancer Res. 1995;55:5276–5282. PMID: 7585588
9. Myatt N, Cree IA, Kurbacher CM, Foss AJ, Hungerford JL, Plowman PN. The ex vivo chemosensitivity profile of choroidal melanoma. Anticancer Drugs. 1997;8:756–762. PMID: 9396619
10. Cree IA, Neale MH, Myatt NE, de Takats PG, Hall P, Grant J, et al. Heterogeneity of chemosensitivity of metastatic cutaneous melanoma. Anticancer Drugs. 1999;10:437–444. PMID: 10477162
11. Breidenbach M, Rein D, Schmidt T, Heindel W, Kolhagen H, Mallmann P, et al. Intra-arterial mitoxantrone and paclitaxel in a patient with Stewart-Treves syndrome: selection of chemotherapy by an ex vivo ATP-based chemosensitivity assay. Anticancer Drugs. 2000;11:269–273. PMID: 10898542
12. Breidenbach M, Rein DT, Mallmann P, Kurbacher CM. Individualized long-term chemotherapy for recurrent ovarian cancer after failing high-dose treatment. Anticancer Drugs. 2002;13:173–176. PMID: 11901311
13. O'Meara AT, Sevin BU. Predictive value of the ATP chemosensitivity assay in epithelial ovarian cancer. Gynecol Oncol. 2001;83:334–342. PMID: 11606094
14. Cree IA, Kurbacher CM, Untch M, Sutherland LA, Hunter EM, Subedi AM, et al. Correlation of the clinical response to chemotherapy in breast cancer with ex vivo chemosensitivity. Anticancer Drugs. 1996;7:630–635. PMID: 8913430
15. Kawamura H, Ikeda K, Takiyama I, Terashima M. The usefulness of the ATP assay with serum-free culture for chemosensitivity testing of gastrointestinal cancer. Eur J Cancer. 1997;33:960–966. PMID: 9291821
16. Sharma S, Neale MH, Di Nicolantonio F, Knight LA, Whitehouse PA, Mercer SJ, et al. Outcome of ATP-based tumor chemosensitivity assay directed chemotherapy in heavily pre-treated recurrent ovarian carcinoma. BMC Cancer. 2003;3:19PMID: 12841853
17. Konecny G, Crohns C, Pegram M, Felber M, Lude S, Kurbacher C, et al. Correlation of drug response with the ATP tumorchemosensitivity assay in primary FIGO stage III ovarian cancer. Gynecol Oncol. 2000;77:258–263. PMID: 10785475
18. Kang HJ, Ko CD, Yoon HS, Kim MB, Ahn SH. The Reliability of histoculture drug response assay (HDRA) in chemosensitivity test for breast cancer. Cancer Res Treat. 2001;33:392–397.
19. In : DeVita VT, Hellman S, Rosenberg SA, editors. Principles and practice of oncology. 2001. 6th edPhiladelphia: Lippincott Williams & Wilkins; p. 303.
20. Cortazar P, Johnson BE. Review of the efficacy of individualized chemotherapy selected by in vitro drug sensitivity testing for patients with cancer. J Clin Oncol. 1999;17:1625–1631. PMID: 10334552
21. Ng TY, Ngan HY, Cheng DK, Wong LC. Clinical applicability of the ATP cell viability assay as a predictor of chemoresponse in platinum-resistant epithelial ovarian cancer using nonsurgical tumor cell samples. Gynecol Oncol. 2000;76:405–408. PMID: 10684718
22. Reinhold U, Tilgen W. Chemosensitivity testing in oncology. 2003. Heidelberg: Springer-Verlag; p. 126–145.
23. Yamaue H, Tanimura H, Tsunoda T, Tani M, Iwahashi M, Noguchi K, et al. Chemosensitivity testing with highly purified fresh human tumour cells with the MTT colorimetric assay. Eur J Cancer. 1991;7:1258–1263. PMID: 1835595
24. Maehara Y, Kusumoto H, Kusumoto T, Anai H, Sugimachi K. Tumor tissue is more sensitive to mitomycin C, carboquone, and aclacinomycin A than is adjacent normal tissue in vitro. J Surg Oncol. 1989;40:4–7. PMID: 2909804
Fig. 13p deletion analysis according to the cancer cell fractionation. 3p deletion analysis was performed using D3S1611 in patient 2. The degree of 3p deletion increased according to the immunomagnetic separation. This result indicates that adequate cancer cell fractionation was achieved. 
Fig. 2Cytotoxic effect of 7 anticancer drugs. A scatter gram shows the heterogeneity of the chemosensitivity for anticancer drugs in the indicated number of lung cancer patients. A broad range of chemosensitivity to the same concentration of anticancer drug was noted. 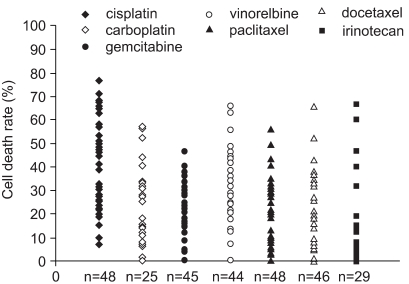
Table 2LOH analysis of the 3p deletion in two lung cancer patients, both before and after cancer cell fractionation 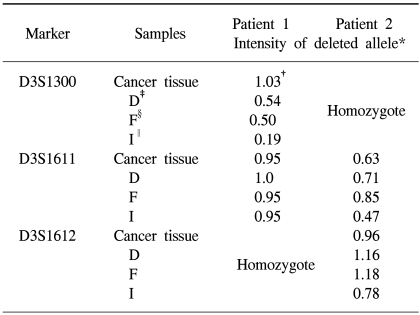 *The intensity denotes the amplified product of the deleted allele from cancer cells and the non deleted allele from contaminated normal cells. Therefore, the lower values indicate a decrease in the proportion of contaminated normal cells. †unit = signal intensity of deleted allele / signal intensity of normal allele ‡after disaggregation, §after ficoll gradient centrifugation, ∥after immunomagnetic separation. |
|
||||||||||||||||||||||||||||||||||||