AbstractPurposeHollow fiber assays offer an early in vivo method of anticancer drug screening. The assays have been optimized for human cancers originating from the lung, breast, colon, ovary, and brain, but not from the stomach and liver. The current study focused on optimization of hollow fiber assays for gastric and hepatocellular carcinoma cell lines.
Materials and MethodsGastric (SNU-16, SNU-484, SNU-668) and hepatocellular (HepG2, SK-Hep-1, Hep3B) carcinoma cell lines in hollow fibers were transplanted subcutaneously and intraperitoneally into mice, which were subsequently treated with a standard anticancer agent, paclitaxel. The hollow fiber activity of paclitaxel in each cell line was compared with the xenograft activity.
ResultsUsing optimized inoculation densities and schedules, treatment with paclitaxel was effective in gastric carcinoma cell lines, SNU-16 and SNU-484, but not in SNU-668. In the hollow fiber assays, paclitaxel was effective in hepatocellular carcinoma cell lines, HepG2 and SK-Hep-1, but not in Hep3B. Consistent with the results of the hollow fiber assay, SNU-16 and SNU-484, but not SNU-668, showed tumor regression, and HepG2 and SK-Hep-1, but not Hep3B, showed effective tumor responses following treatment with paclitaxel in xenograft models. When EW7197, a novel compound, and flavopiridol were tested in SNU-16 cells under optimized conditions, the hollow fiber activity showed good correlation with the xenograft activity of each compound.
IntroductionSeveral preclinical in vitro and in vivo tumor models based on human cancer cell lines are being used for discovery and evaluation of new anticancer drugs. Many in vitro tumor models cannot replicate the complex tumor microenvironment and pharmacokinetics of drugs in vivo, therefore, a demonstration of in vivo drug efficacy is required after the in vitro screening process [1,2]. The xenograft mouse model is the conventional method used for preclinical in vivo drug testing, however, it requires significant numbers of mice and quantities of test compounds and incurs high costs in terms of both labor and time [2]. In addition, some human cancer cell lines do not readily form tumors in animals [2].
Hollow fiber assays, developed by the National Cancer Institute (NCI) in the United States to facilitate drug screening and development [3], are used in characterization of the in vivo activities of small organic compounds before xenograft testing is undertaken. The hollow fiber assay is based on techniques for cultivation of mammalian cells in hollow fibers permeable to substances with a molecular weight<500,000 Da, and implantation of the fibers in various body compartments of mice, followed by drug exposure and quantitation of the viability of the cells [3]. Hollow fiber assays can test multiple tumor cell samples in two physiological compartments (subcutaneously and intraperitoneally) within one mouse, enabling effective pairing of a novel compound with an appropriate cell line. Compared with the traditional xenograft model, this assay reduces the time required for completion of testing and reduces costs by using fewer mice and lower quantities of compounds; it also facilitates in vivo analysis of the effects of drugs on human cancer cell lines that do not form tumors in animals and shows high correlation with the xenograft assay [4,5,6]. In addition, it can aid in estimating the doses of test compounds and the administration routes for more extensive in vivo testing [3]. This assay cannot replace human xenograft models because it does not fully reflect the complex interaction between the host and human cancer cells, however, it is useful as a prescreen before labor-intensive, expensive, and time-consuming xenograft testing is undertaken [2].
Stomach and liver cancers are the most common cancers and a major cause of cancer deaths worldwide [7,8]. Hollow fiber assays have been optimized for human cancers originating from the lung, breast, colon, ovary, and brain, but not from the stomach and liver [3]. Therefore, the purpose of the current study was to optimize hollow fiber assays for human gastric and hepatocellular carcinoma cell lines.
Materials and Methods1. MiceSeven-week-old female Balb/C (nu/nu) mice and female nonobese diabetic/severe combined immunodeficiency (NOD/SCID) mice were purchased from Orient Bio (Seongnam, Korea). The mice were housed five per cage in a clean rack maintained at room temperature (22-26℃) under a 12-hour light/dark illumination cycle. On the day they were scheduled for sacrifice, the mice were anesthetized with isoflurane and sacrificed by cervical dislocation. All of the experiments were performed in accordance with the Guide for the Care and Use of Laboratory Animals of the National Cancer Center (NCC) and approved by the NCC Animal Care Committee (approval number: NCC-12-050E).
2. Cell linesThe human gastric cancer cell lines, SNU-16, SNU-484, and SNU-668, were purchased from Korean Cell Line Bank (KCLB, Seoul, Korea). The human liver cancer cell lines, SK-Hep-1, HepG2, and Hep3B, were obtained from American Tissue Culture Collection (ATCC, Manassas, VA). All of the cancer cell lines were adapted to RPMI 1640 (WelGENE, Daegu, Korea) containing 10% fetal bovine serum (FBS) (WelGENE) and maintained as monolayer cultures at 37℃ in a humidified, 5% CO2 environment.
3. DrugsTwo anticancer drugs, paclitaxel and flavopiridol, were purchased from Sigma Aldrich (Buchs, Switzerland). The drugs were dissolved in 10% dimethyl sulfoxide (DMSO). The mice received intraperitoneal injection with paclitaxel (30 mg/kg) or flavopiridol (5 mg/kg) four times daily for the hollow fiber assays and five times daily for the xenograft assays. Mice in a vehicle control group received 10% DMSO in saline. EW7197 (US patent 8080568), a novel small organic compound, was kindly provided by Dr. Dae-Kee Kim [9]. This compound was administered orally to mice using the gavage technique at a dose of 40 mg/kg four times daily for the hollow fiber assay and five times daily for the xenograft assay.
4. Hollow fiber assayEach mouse received six polyvinylidene fluoride (PVDF) hollow fibers (S9320101, Spectrum Laboratories, Rancho Dominquez, CA), representing three stomach or liver cancer cell lines, subcutaneously and intraperitoneally, as described previously [3]. There were three mice per paclitaxel-treated group and three mice per vehicle control group. Briefly, PVDF hollow fibers with inner diameters of 1.0 mm and a molecular weight cutoff of 500 kDa were individually flushed and incubated in 70% ethanol at room temperature for at least 72 hours. After washing with deionized water, the fibers were autoclaved and flushed with RPMI 1640 containing 20% FBS. The cell lines were harvested with trypsin/ethylenediaminetetraacetic acid, pelleted by centrifugation, resuspended in conditioned medium, and diluted with RPMI 1640 containing 20% FBS. The optimal cell suspension density showing linearity in the growth of each cell line in the fibers during the experimental periods is shown in Table 1. The fibers were filled with the cell suspensions using a 20-gauge needle. Each fiber was then heat sealed by clamping preheated smooth-jawed needle-holders across the fiber every 2 cm along its length. The samples were incubated for one, two, or three nights depending on the growth potential of each cell line in the fiber at 37℃ in a 5% CO2 incubator prior to implantation into 7- to 10-week-old female Balb/C (nu/nu) mice. The implantation was performed while the mice were under inhalational isoflurane anesthesia on day 0. Three subcutaneous fibers containing the three stomach or three liver cancer cell lines were implanted by caudal insertion of a trocar containing fibers through a skin incision made at the nape of the neck. Three intraperitoneal fibers containing the three stomach or the three liver cancer cell lines were also inserted into the peritoneal cavity of the same mice in a craniocaudal direction using an incision through the abdominal wall. Two layers of sutures were used to close the abdominal incision. To identify the growth potential of the cell line, the viable cell mass in the fibers was estimated on day 5. In vitro control fibers were also prepared and incubated in the same media during the experiment.
Drug treatment started three or four days after implantation of the hollow fiber according to the growth potential of each cell line in the fiber following implantation. The drugs were administered once daily for four days. The mice were sacrificed one day after the last drug treatment. MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyletrazolium bromide) dye conversion assays were performed in order to define the viable cell mass within the fiber, as described previously [3]. The hollow fiber activity of the agents was defined as the changes in the viable cell mass in fibers from compound-treated and vehicle-treated mice.
To determine whether the hollow fiber conditions were optimized, we tested two chemical compounds, EW7197 and flavopiridol, using SNU-16 human stomach cancer cells. EW7197 and flavopiridol were administered orally and intraperitoneally, respectively.
5. Xenograft assayThe tumor cells lines (107 cells in 100 µL of serum-free RPMI) were mixed with equal volumes of Matrigel (BD Biosciences, Bedford, MA) and injected into the subcutaneous flank tissue of NOD/SCID mice. Once formed, the tumors were harvested and fragmented into 3 mm tissue sections and serially transplanted into the subcutaneous flank tissue of a larger number of NOD/SCID mice for examination of the xenograft activity of the drugs. All subsequent experiments were performed during the third (SNU-16, SNU-668, SK-Hep-1, HepG2, and Hep3B) or fourth (SNU-484) in vivo passage. The tumor volume (V) was calculated using the following equation: V=1/2×a×b2, where a and b are the longest and the shortest diameters of the tumor mass (in millimeters), respectively [6]. When the tumors reached approximately 100 mm3, mice harboring tumors of similar sizes were staged using random numbers generated using SAS ver. 9.1.3 (SAS Institute Inc., Cary, NC). There were three mice per drug-treated group and three mice per vehicle control group. After staging, either the drugs or the vehicle control was given to the mice for five consecutive days at the same dose and by the same routes used in the hollow fiber assay.
Responses of the tumors to the drugs were evaluated using percent treated/control (% T/C), as determined by dividing the median tumor volume of the treatment group (T) by that of the negative control group (C) on the day of measurement. If a tumor showed regression, % T/C was defined as the negative of the percentage of decrease in the median tumor volume of the treatment group (T) relative to the baseline volume on the day of measurement. The optimal (minimum) value of % T/C during the first seven days of treatment was used to quantify the xenograft activity of the drugs in each cell line xenograft.
6. Statistical analysisAny statistically significant difference was compared using the unpaired two-tailed Student's t-test. In addition, Pearson's correlation test was used to examine the association between the activities of the hollow fiber and those of the xenograft. Statistical analysis was performed using Prism 4.0 ver. 4.0 (GraphPad Software, San Diego, CA). A p-value less than 0.05 was considered statistically significant.
ResultsDue to the difference in the growth potential inside the fibers of each cell line, the proper density showing continued growth in the fibers during the experimental periods needs to be determined [3]. Using the inoculation densities and the schedules shown in Table 1, all of the cell lines showed continued growth in the fibers until harvesting, as indicated by the larger quantities of viable cell mass in the day 7 and day 8 fibers than in the day 5 fibers of saline-treated mice (data not shown).
Figs. 1 and 2 show the results of the hollow fiber and the xenograft assay of the stomach and liver cancer cell lines. SNU-16 and SNU-484, but not SNU-668, showed decreases of greater than 50% in viable cell masses within the intraperitoneal hollow fibers following treatment with paclitaxel, and HepG2 and SK-Hep-1 showed a decrease of 57% and 35%, respectively. Hep3B showed no difference in viable cell masses within the intraperitoneal hollow fibers following treatment with paclitaxel, and the treatment had less dramatic effects on all of these cells in the subcutaneous hollow fibers. This finding is consistent with the pharmacokinetics of paclitaxel reported in other cell lines [3,4,5].
All of the cell lines readily formed xenograft tumors in the subcutaneous flank tissues of NOD/SCID mice (100% take rates [5/5] in all cell lines). The SNU-16 and SNU-484 cell lines, but not the SNU-668 cell line, showed tumor regression following treatment with paclitaxel, with positive xenograft activities of -60% and -70%, respectively. Although these cell lines did not show tumor regression, effective tumor responses were observed in HepG2 and SK-Hep-1, but not Hep3B, following treatment with paclitaxel.
Tables 2 and 3 show the correlations between the hollow fiber assay and the xenograft assay. Consistent with the results of the intraperitoneal hollow fiber assay, SNU-16, SNU-484, HepG2, and SK-Hep-1, exhibiting positive hollow fiber activities, showed effective tumor responses to paclitaxel in the xenograft cell lines. Paclitaxel did not exhibit significant xenograft activity against the SNU-668 and Hep3B cell lines. This finding is consistent with paclitaxel not showing significant hollow fiber activity in these cell lines. The xenograft activities of paclitaxel showed good correlation with the intraperitoneal hollow fiber activities (Pearson correlation, 0.94) in the stomach cancer cell lines and with the intraperitoneal hollow fiber activities (Pearson correlation, 0.99) in the hepatocellular carcinoma cell lines.
DiscussionIn routine hollow fiber screening, the US NCI Developmental Therapeutics Program uses a standard panel of 12 tumor cell lines, representing six different histologies, selected according to the expected behavior of their corresponding xenograft. The cell lines include NCI-H23 and NCI-H522 (non-small cell lung), MDA-MB-231 and MDA-MB-435 (breast), SW-620 and COLO 205 (colon), LOX and UACC-62 (melanoma), OVCAR-3 and OVCAR-5 (ovary), and U251 and SF-295 (glioma) [3]. These cells, at densities of 2-10×106 cells/mL depending on the growth potential in the hollow fibers of the cell lines, are placed in hollow fibers, which are inserted into peritoneal cavities and subcutaneous tissues of mice. The mice receive intraperitoneal injection with one of two doses of the experimental compounds, vehicle controls, or a positive control. This assay is validated using standard anticancer agents and should show positive hollow fiber activities as those agents with a 50% or more reduction of the vehicle control. Due to its broad spectrum of antitumor activities, paclitaxel is used as a positive control in hollow fiber assays [10,11]. Experimental compounds were considered to have an effect on a particular fiber if there was a 50% or greater reduction compared with the vehicle controls [3]. Compounds showing positive hollow fiber activity were considered for a follow-up xenograft test.
In the current study, the SNU-16 and SNU-484 stomach cancer cell lines showed a reduction in net growth of greater than 50% in paclitaxel-treated samples compared to vehicle control samples at the densities and schedules described herein. The HepG2 and SK-Hep-1 hepatocellular carcinoma cell lines showed a reduction of 57% and 35%, respectively. These cells formed xenografts in nude mice, and the xenograft activities of paclitaxel in these cells showed good correlation with the hollow fiber activities.
The biological and molecular characteristics of these cells were previously characterized [12,13,14,15,16]. Briefly, SNU-16 grows as floating cells and has MYC gene amplification [12,13,15], and SNU-484 grows as a monolayer and contains mutant p53 [14]. SK-Hep-1 has an endothelial origin and expresses both vascular endothelial growth factor receptor-2 and fibroblast growth factor receptor 1 [16]. HepG2 is often used as a tool for screening the cytotoxicity of novel compounds because it is well differentiated and shares many of the genotypic features of normal hepatocytes [17,18].
EW7197, another small organic compound, and flavopiridol were used in validation of our hollow fiber assay protocols. EW7197, a 2-pyridyl substituted imidazole, is a therapeutic ALK5 inhibitor targeting cancer metastasis [9]. As EW7197 inhibits the transforming growth factor-β signaling pathway, it was expected not to exhibit any hollow fiber activities. In contrast, flavopiridol is a cyclin-dependent kinase inhibitor targeting cancer cell proliferation. Given its proven in vivo antitumor activity [19], flavopiridol was used as the positive control in the hollow fiber assay. At a biologically effective dose, EW7197 did not exhibit any hollow fiber activity in the SNU-16 cell line. Consistent with the results of the hollow fiber assay, this compound also did not exhibit xenograft activity, whereas flavopiridol exhibited significant xenograft and hollow fiber activity in the SNU-16 cell line (Fig. 3). These results validate the utility of the stomach cancer hollow fiber assay protocol proposed in this paper.
In summary, we report on optimized hollow fiber assay protocols for gastric cancer and hepatocellular carcinoma cell lines. The hollow fiber assay protocols can be used for comparison of the efficacy of novel small molecules and paclitaxel. Compared with xenograft assays, hollow fiber assays save time (1-2 weeks vs. 4-6 weeks) and resources while still predicting the xenograft activity of candidate small molecules. Therefore, our protocols may be useful for screening candidate small molecules that may be active against gastric cancer and hepatocellular carcinoma, both of which are common in Korea.
ConclusionAlthough stomach and liver cancers are the most common cancers and a major cause of cancer-related deaths worldwide, the standard hollow fiber assay panels do not include these cancers. We have established the optimal conditions for this assay using well-characterized gastric and hepatocellular carcinoma cell lines. The hollow fiber assay activities showed high correlation with those of the xenograft. Our protocols may be useful for screening candidate small molecules that may be active against gastric cancer and liver cancers, both of which are common in Korea.
AcknowledgmentsThe work was supported by National Cancer Center Grants 1111370-1/1210051 and by the Proteogenomic Research Program and 2013K000429 funded by the Korean Ministry of Science, ICT, and Future Planning. The authors would like to thank Dr. Hollingshead at the US National Cancer Institute for training the authors for use of hollow fiber assay techniques.
References1. Phillips RM, Bibby MC, Double JA. A critical appraisal of the predictive value of in vitro chemosensitivity assays. J Natl Cancer Inst. 1990;82:1457–1468. PMID: 2202838
2. Sharma SV, Haber DA, Settleman J. Cell line-based platforms to evaluate the therapeutic efficacy of candidate anticancer agents. Nat Rev Cancer. 2010;10:241–253. PMID: 20300105
3. Hollingshead MG, Alley MC, Camalier RF, Abbott BJ, Mayo JG, Malspeis L, et al. In vivo cultivation of tumor cells in hollow fibers. Life Sci. 1995;57:131–141. PMID: 7603295
4. Hall LA, Krauthauser CM, Wexler RS, Hollingshead MG, Slee AM, Kerr JS. The hollow fiber assay: continued characterization with novel approaches. Anticancer Res. 2000;20:903–911. PMID: 10810375
5. Johnson JI, Decker S, Zaharevitz D, Rubinstein LV, Venditti JM, Schepartz S, et al. Relationships between drug activity in NCI preclinical in vitro and in vivo models and early clinical trials. Br J Cancer. 2001;84:1424–1431. PMID: 11355958
6. Lee KH, Rhee KH. Correlative effect between in vivo hollow fiber assay and xenografts assay in drug screening. Cancer Res Treat. 2005;37:196–200. PMID: 19956503
7. Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Park EC, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2008. Cancer Res Treat. 2011;43:1–11. PMID: 21509157
8. Jemal A, Center MM, DeSantis C, Ward EM. Global patterns of cancer incidence and mortality rates and trends. Cancer Epidemiol Biomarkers Prev. 2010;19:1893–1907. PMID: 20647400
9. Kim SW, Kim SJ, Park SA, Kim MJ, Kim DK, Sheen YY. Anti-metastasis effect of EW-7197, a novel ALK5 inhibitor in both breast cancer cells in vitro and mouse model in vivo. Cancer Res. 2012;72(8 Suppl 1):Abstr 1918.
10. Wani MC, Taylor HL, Wall ME, Coggon P, McPhail AT. Plant antitumor agents. VI. The isolation and structure of taxol, a novel antileukemic and antitumor agent from Taxus brevifolia. J Am Chem Soc. 1971;93:2325–2327. PMID: 5553076
11. Rose WC. Taxol: a review of its preclinical in vivo antitumor activity. Anticancer Drugs. 1992;3:311–321. PMID: 1358264
12. Park JG, Frucht H, LaRocca RV, Bliss DP Jr, Kurita Y, Chen TR, et al. Characteristics of cell lines established from human gastric carcinoma. Cancer Res. 1990;50:2773–2780. PMID: 2158397
13. Bar-Am I, Mor O, Yeger H, Shiloh Y, Avivi L. Detection of amplified DNA sequences in human tumor cell lines by fluorescence in situ hybridization. Genes Chromosomes Cancer. 1992;4:314–320. PMID: 1377938
14. Park JG, Yang HK, Kim WH, Chung JK, Kang MS, Lee JH, et al. Establishment and characterization of human gastric carcinoma cell lines. Int J Cancer. 1997;70:443–449. PMID: 9033653
15. Kim JH, Takahashi T, Chiba I, Park JG, Birrer MJ, Roh JK, et al. Occurrence of p53 gene abnormalities in gastric carcinoma tumors and cell lines. J Natl Cancer Inst. 1991;83:938–943. PMID: 1676761
16. Heffelfinger SC, Hawkins HH, Barrish J, Taylor L, Darlington GJ. SK HEP-1: a human cell line of endothelial origin. In Vitro Cell Dev Biol. 1992;28A:136–142. PMID: 1371504
17. Sassa S, Sugita O, Galbraith RA, Kappas A. Drug metabolism by the human hepatoma cell, Hep G2. Biochem Biophys Res Commun. 1987;143:52–57. PMID: 3030322
18. Mersch-Sundermann V, Knasmuller S, Wu XJ, Darroudi F, Kassie F. Use of a human-derived liver cell line for the detection of cytoprotective, antigenotoxic and cogenotoxic agents. Toxicology. 2004;198:329–340. PMID: 15138059
19. Drees M, Dengler WA, Roth T, Labonte H, Mayo J, Malspeis L, et al. Flavopiridol (L86-8275): selective antitumor activity in vitro and activity in vivo for prostate carcinoma cells. Clin Cancer Res. 1997;3:273–279. PMID: 9815683
Fig. 1Intraperitoneal hollow fiber and xenograft activities of paclitaxel in gastric cancer cells. Error bars are presented as standard deviation. 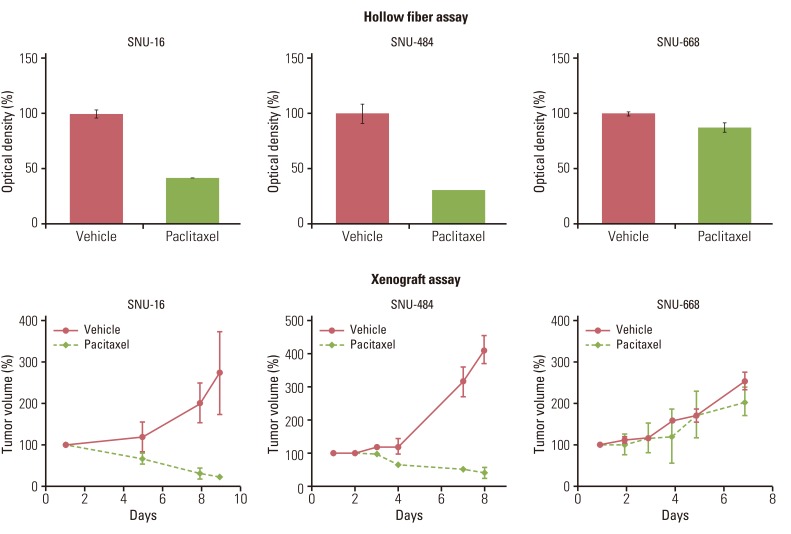
Fig. 2Intraperitoneal hollow fiber and xenograft activities of paclitaxel in hepatocellular carcinoma cells. Error bars are presented as standard deviation. 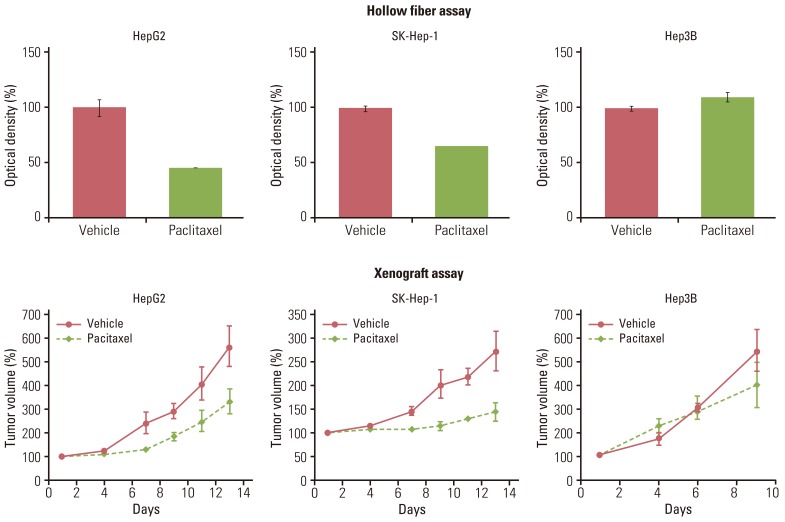
Fig. 3Intraperitoneal hollow fiber and xenograft activities of EW7197 and flavopridol in SNU-16 cells. Error bar are presented as standard deviation. 
Table 1Inoculation density and schedule Table 2Intraperitoneal and subcutaneous HF activities versus xenograft activities in gastric carcinoma cell lines
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||